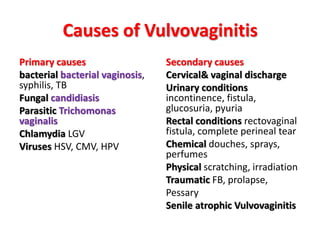
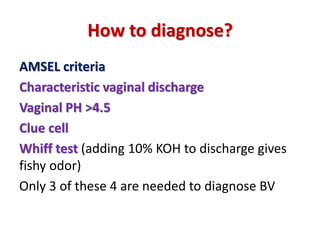
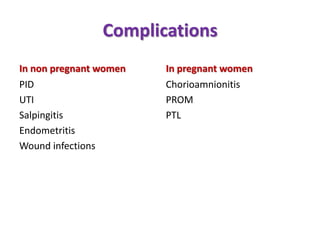
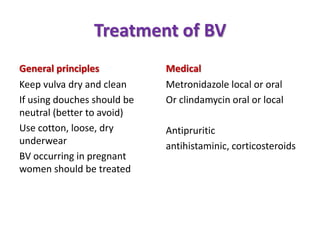
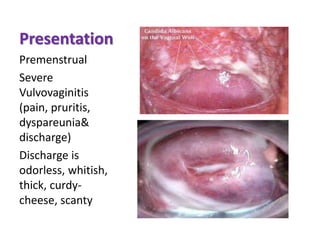
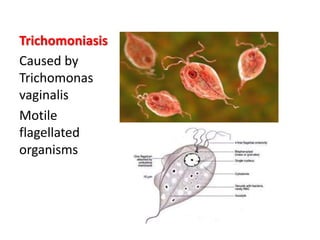
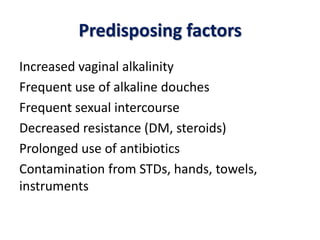
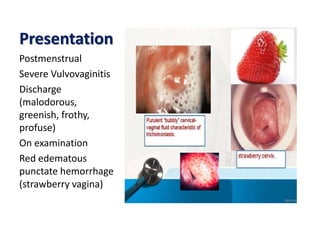
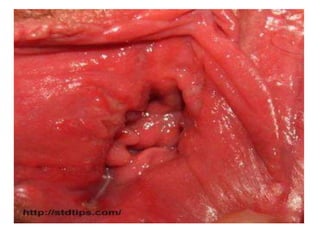
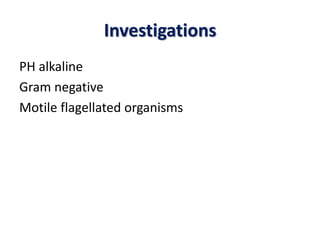
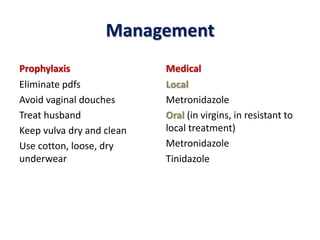
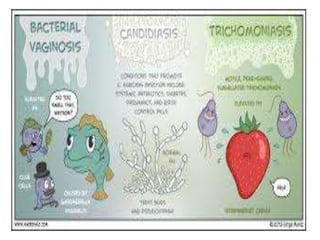
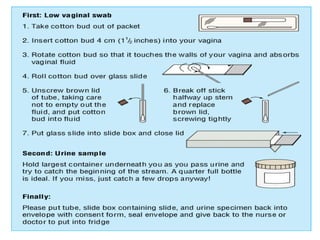
Vulvovaginitis is an inflammation of the vulva and vagina, common in women of all ages and caused by various factors such as bacteria, fungi, and viruses. Key types of vulvovaginitis include bacterial vaginosis, candidiasis, and trichomoniasis, each with specific presentations and treatment methods. Diagnosis typically involves criteria based on symptoms and lab tests, while management focuses on maintaining cleanliness, using appropriate medications, and treating partners.