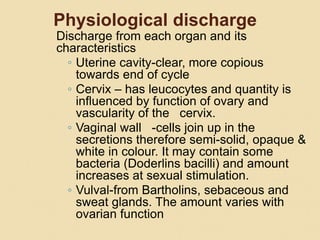
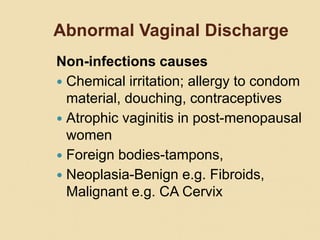
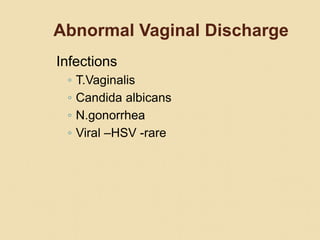
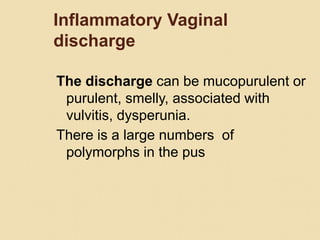
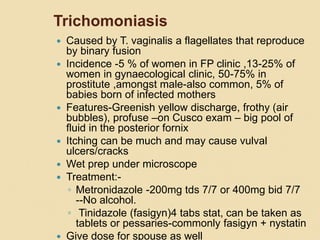
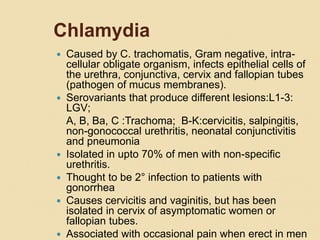
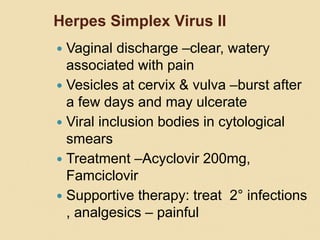
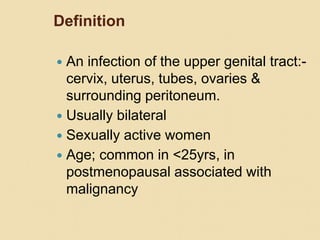
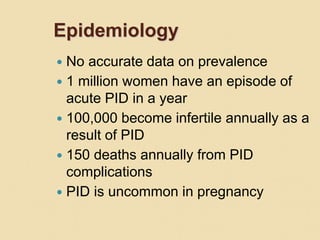
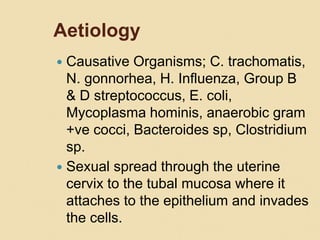
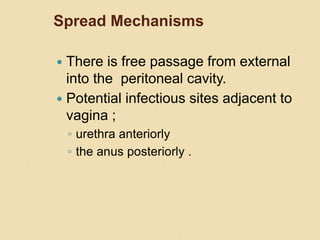
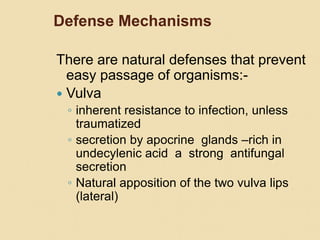
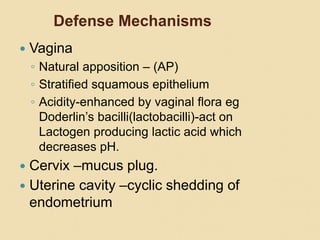
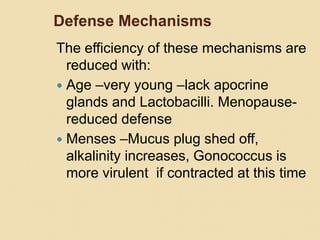
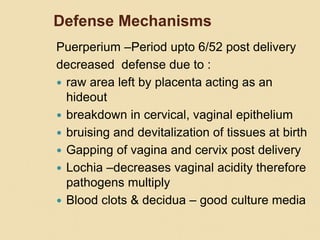
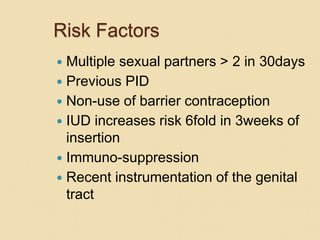
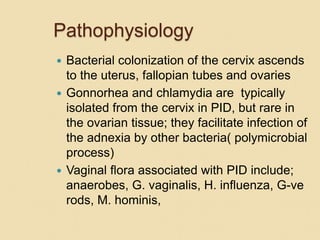
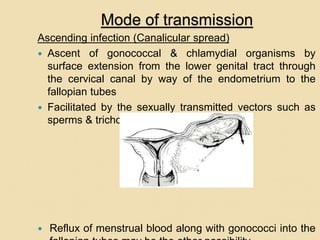
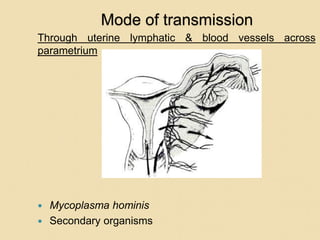
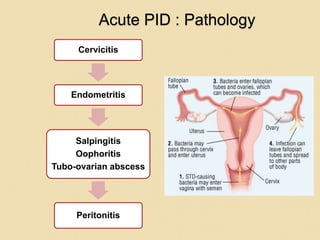
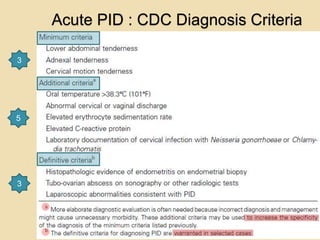
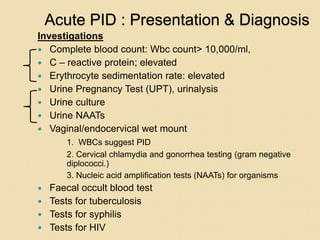
This document discusses sexually transmitted infections and gynaecologic infections. It begins by defining lower genital tract infections and outlining their causes and management. Specific infections discussed include trichomoniasis, candidiasis, gonorrhea, chlamydia, bacterial vaginosis, herpes, HIV, and pelvic inflammatory disease. The document emphasizes the importance of screening, case management using a syndromic approach, and targeted interventions to control sexually transmitted infections.