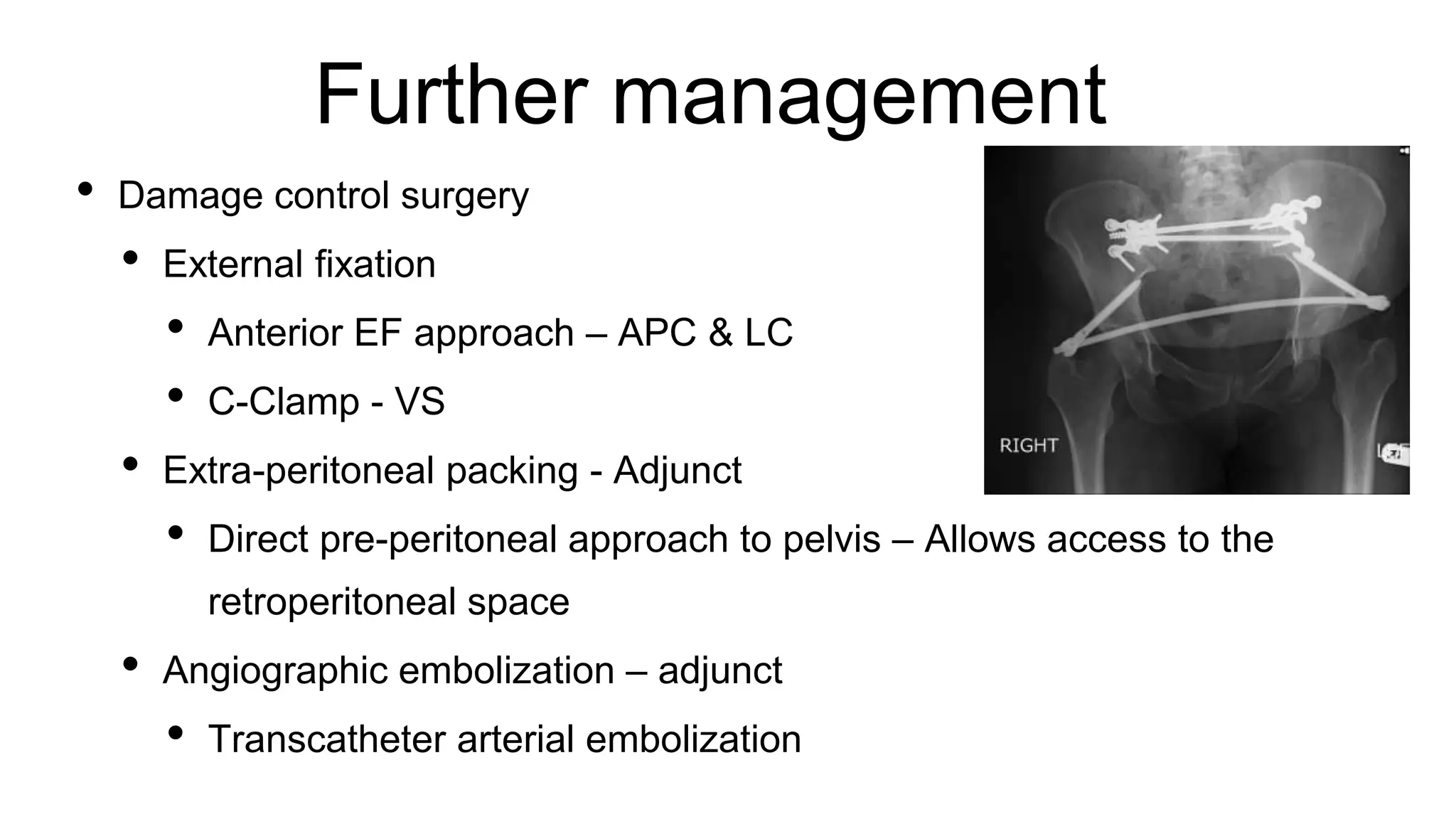
The document outlines the assessment and management of pelvic fractures in emergency medicine, detailing essential aspects like epidemiology, classifications, and treatment protocols. It includes a case study of a 39-year-old male with a pelvic fracture from a motorcycle accident, emphasizing the importance of initial assessment and potential complications. The document also discusses surgical approaches and considerations for managing associated injuries and complications.