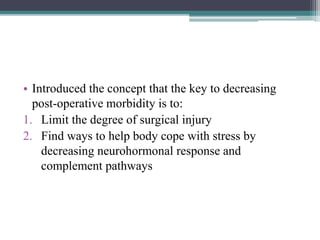
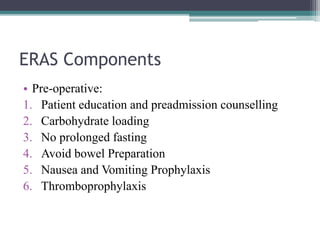
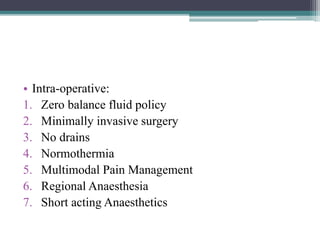
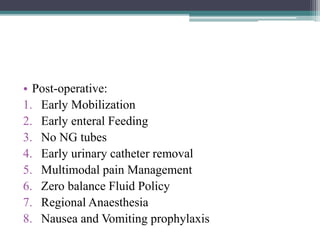
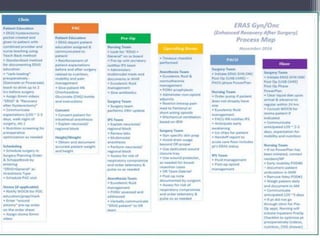
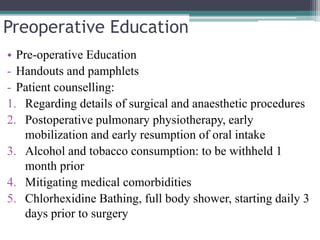
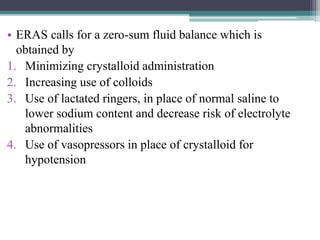
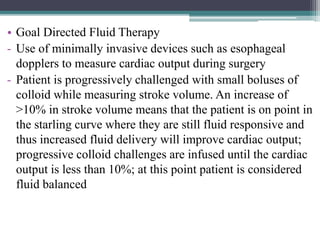
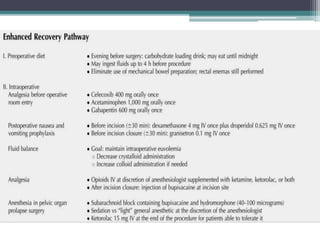
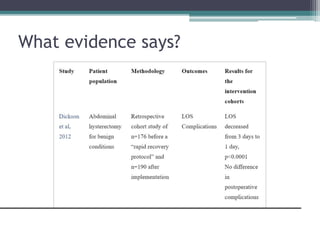
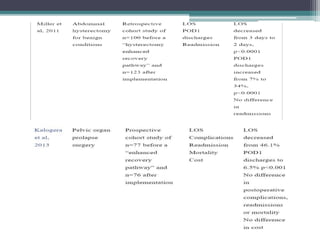
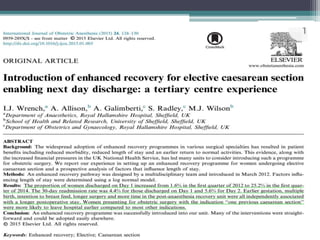
ERAS (Enhanced Recovery After Surgery) is a collection of evidence-based practices designed to improve recovery after major surgery. The goals are to reduce surgical stress, maintain normal physiologic function, and enhance early mobilization. ERAS emphasizes preoperative education, minimizing fasting times, multimodal pain control, early feeding and mobilization to reduce length of stay, complications, and costs while improving patient satisfaction. It was first developed in the 1990s and involves protocols tailored for specific surgeries like gynecologic procedures.