The document discusses rectal prolapse, highlighting its association with other pelvic issues and the evolution of surgical techniques. It emphasizes the lack of high-quality evidence regarding the effectiveness of various surgical approaches and suggests the need for further large-scale studies. The author's conclusions advocate for tailored surgical options based on individual patient conditions while considering risks and recurrence rates.





















































![Indication for rectopexy
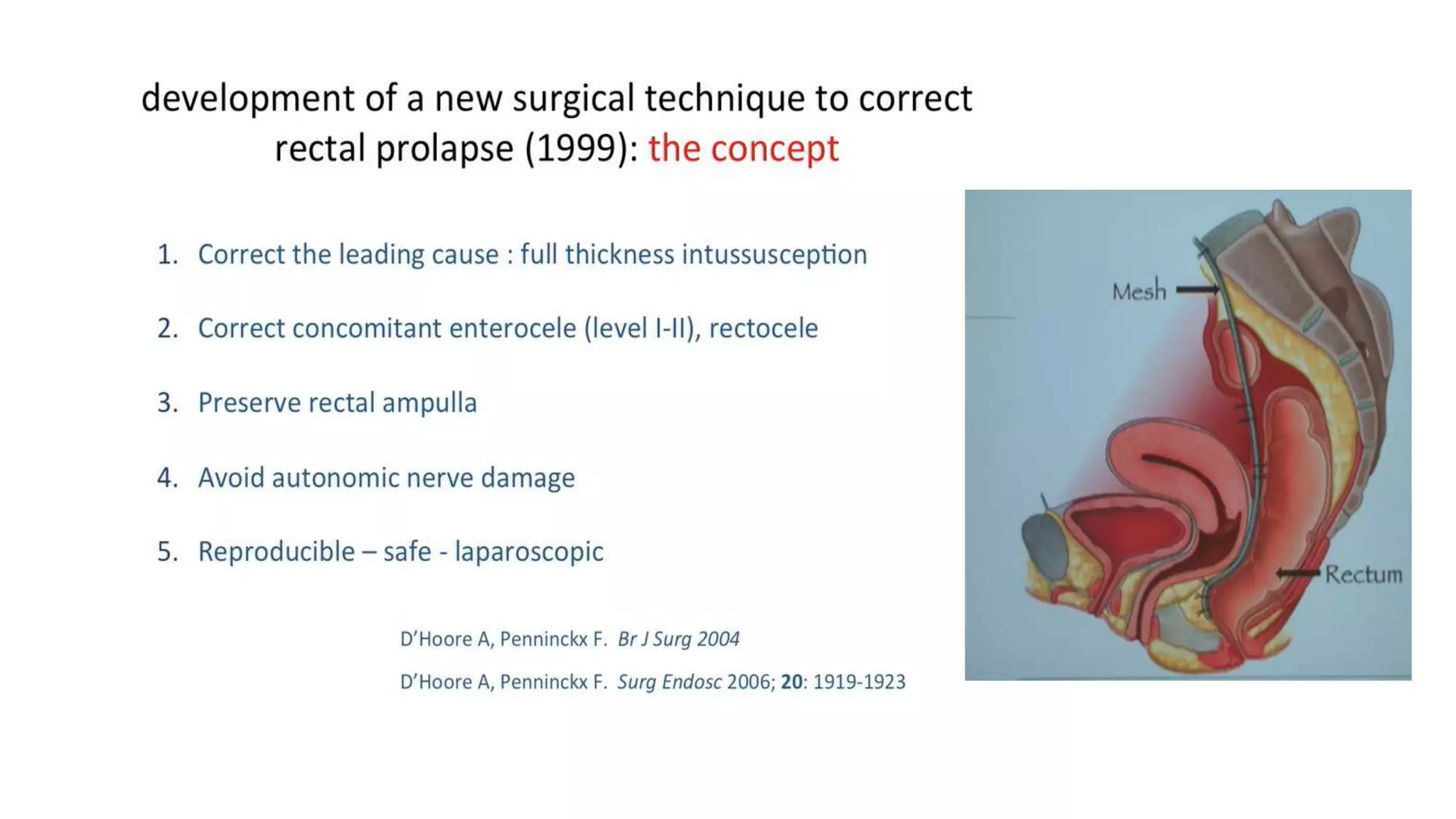
Indications for ventral mesh rectopexy-vaginal sacrocolpopexy.
• Hysterectomy (Vaginal > Total abdominal hysterectomy), vault and/or vaginal prolapse.
• Large cystocele (additional laparoscopic colporraphy)
• Grade IV/V rectal intussusception, grade III enterocele, descending perineum.
• Poor sphincter function.
• External prolapse
• Young men with above and/or solitary rectal ulcer (SRU).
• SRU (Failed STARR), established and fibrotic SRU
• Relapsing symptoms post STARR
Slow transit constipation and internal prolapse
• Any of above (in women) plus urinary stress incontinence or stress incontinence post ventral mesh rectopexy
[additional tension free vaginal tape (TVT)]
• Failed gynecological repairs, Delorme’s, Altemeire, posterior rectopexy, poorly executed ventral rectopexy
Lindsey I, Nugent K, Dixon T. (2010) Pelvic floor disorders for Colorectal Surgeon, Oxford University Press.](https://image.slidesharecdn.com/rectalprolapsedowereallyhaveaperfectsurgicalsolutionpptxcopy-190115154002/75/Rectal-prolapse-Do-we-really-have-a-perfect-surgical-solution-pptx-copy-57-2048.jpg)



