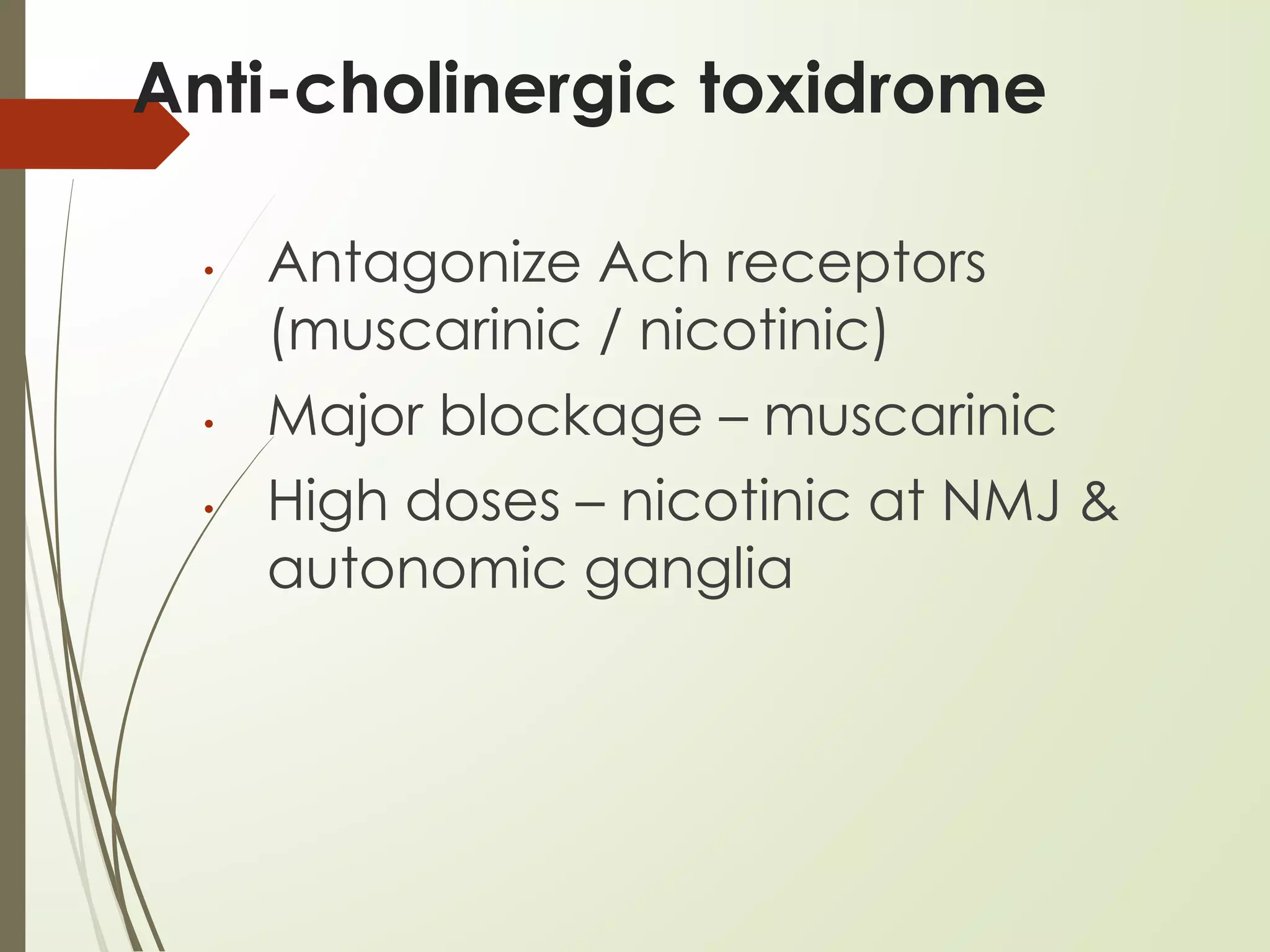
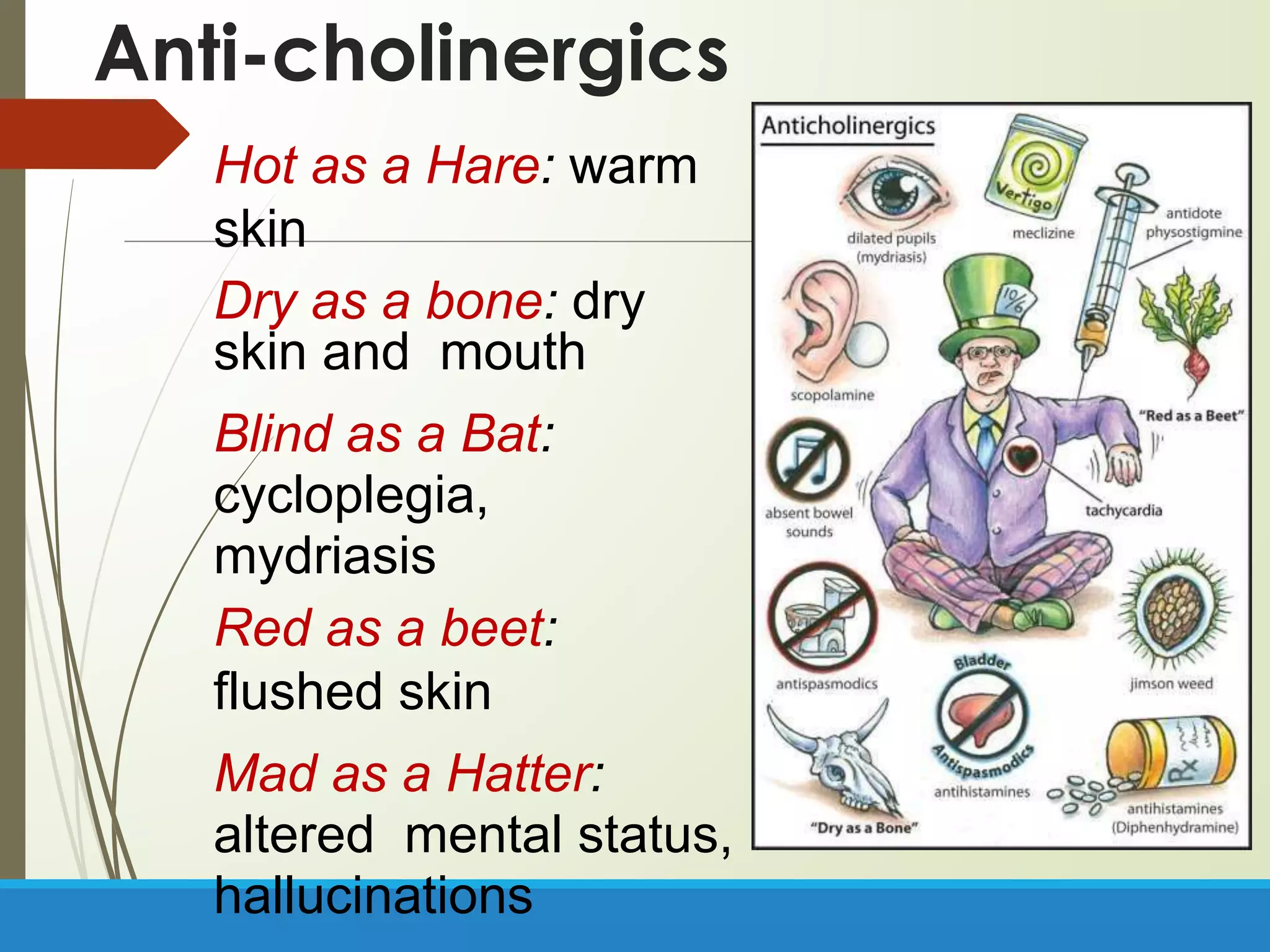
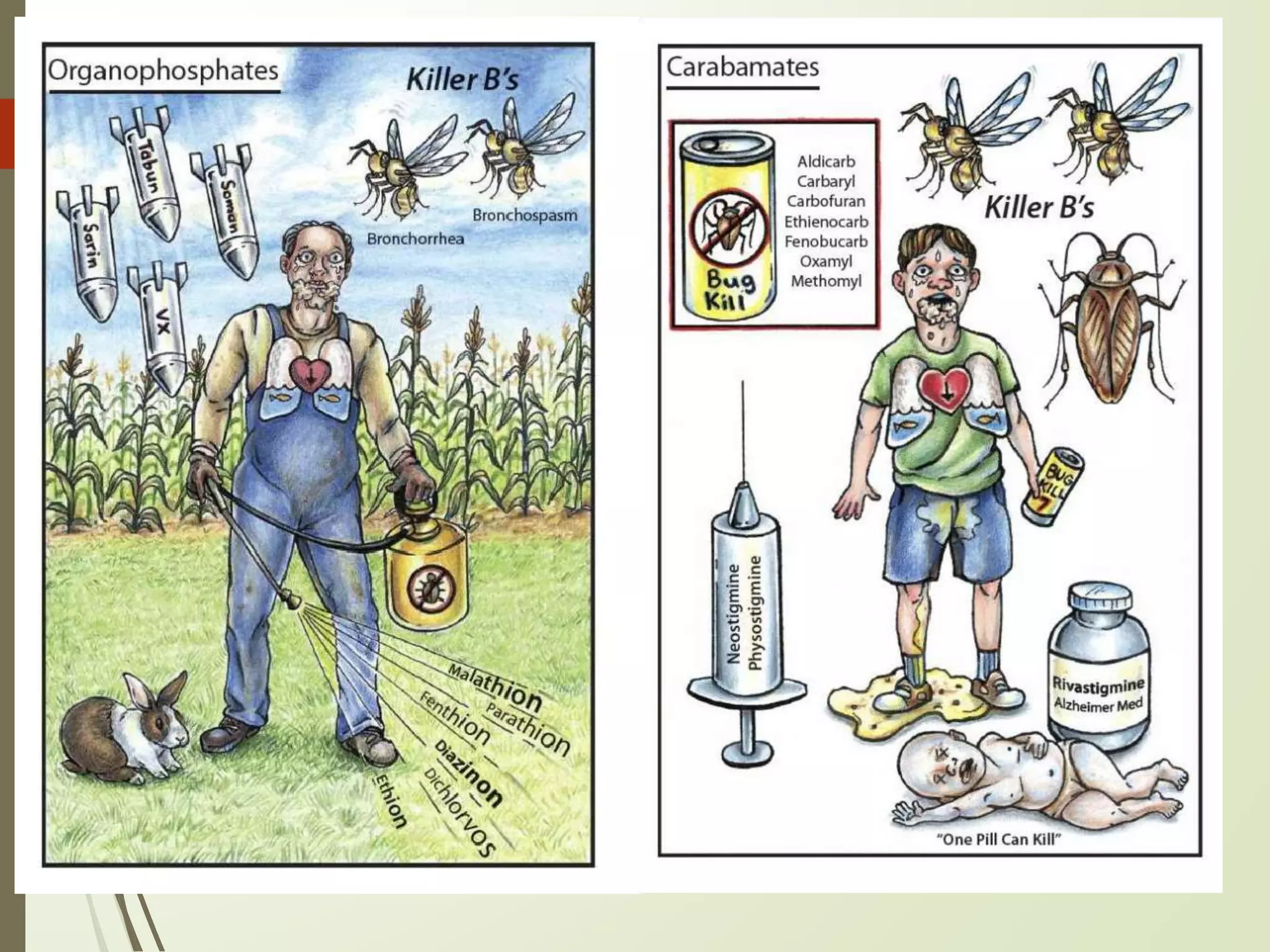
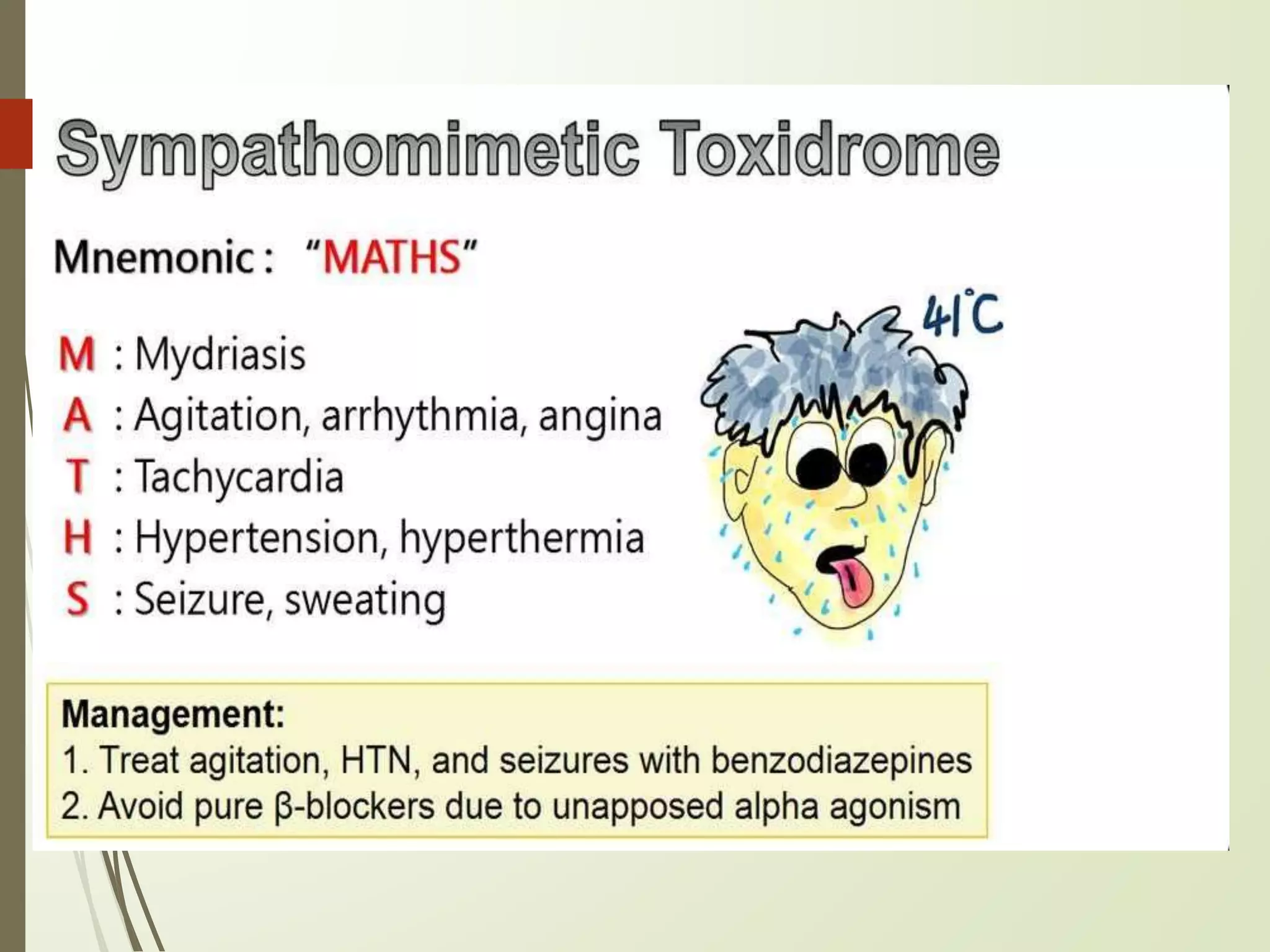
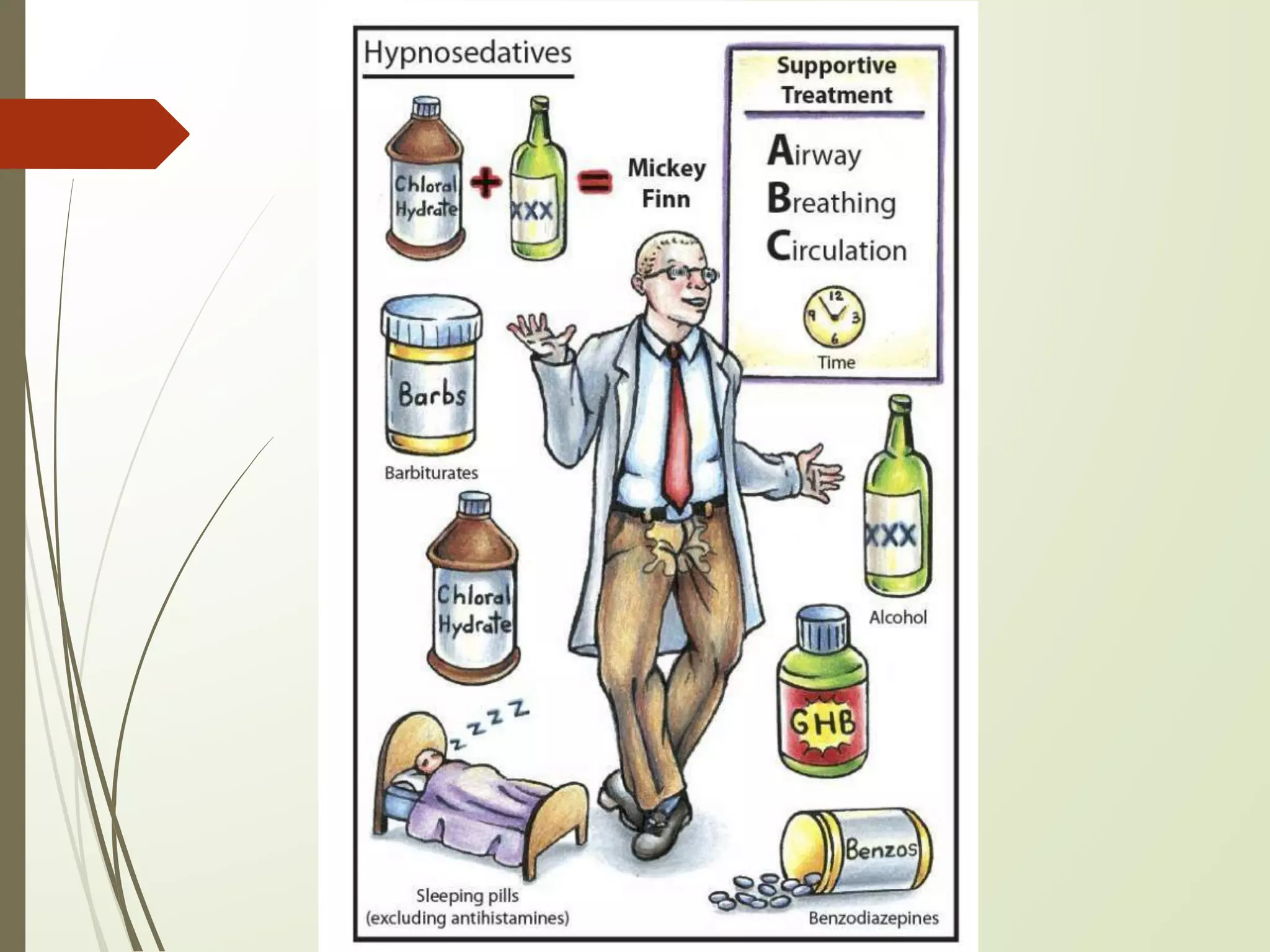
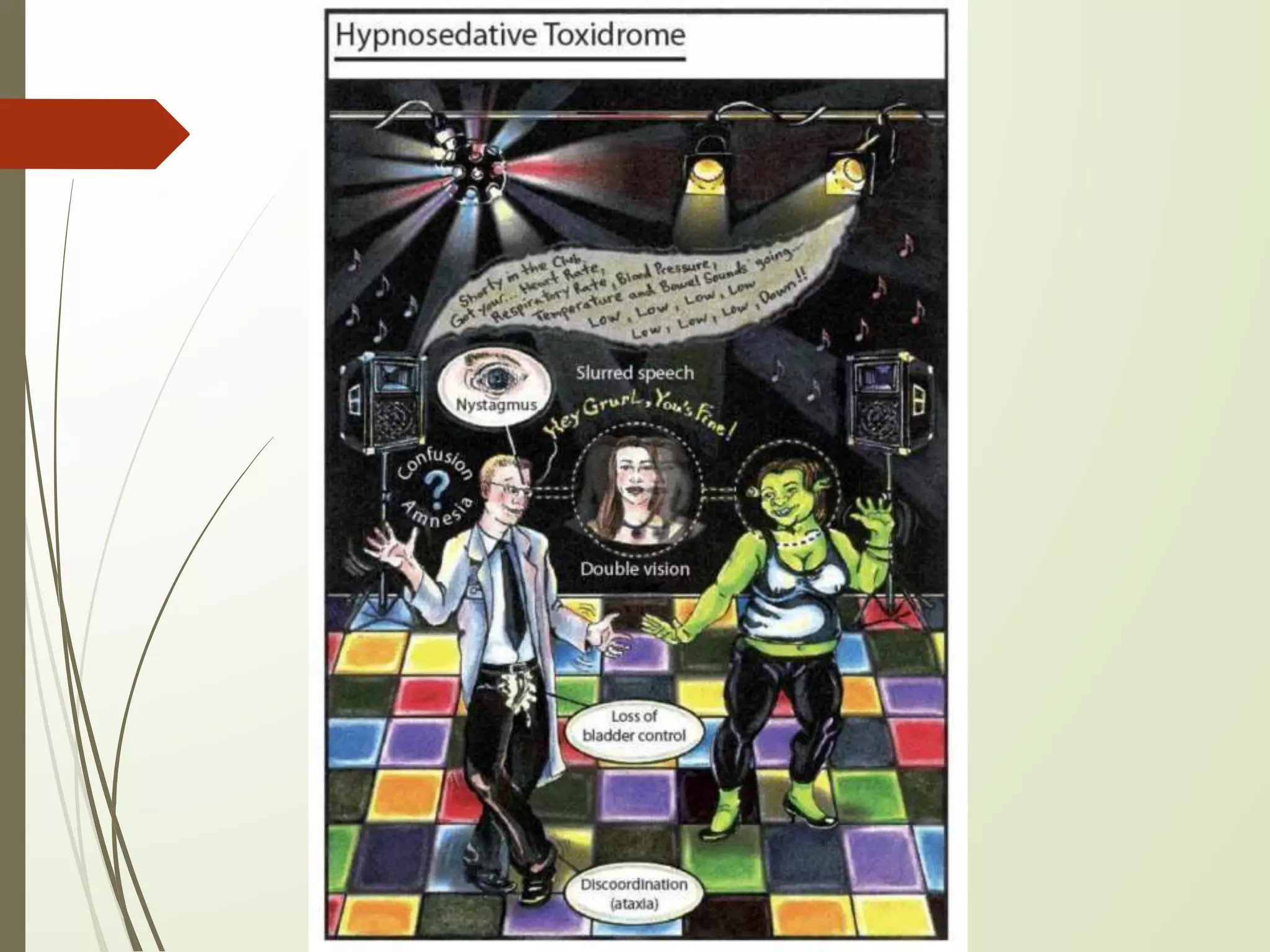
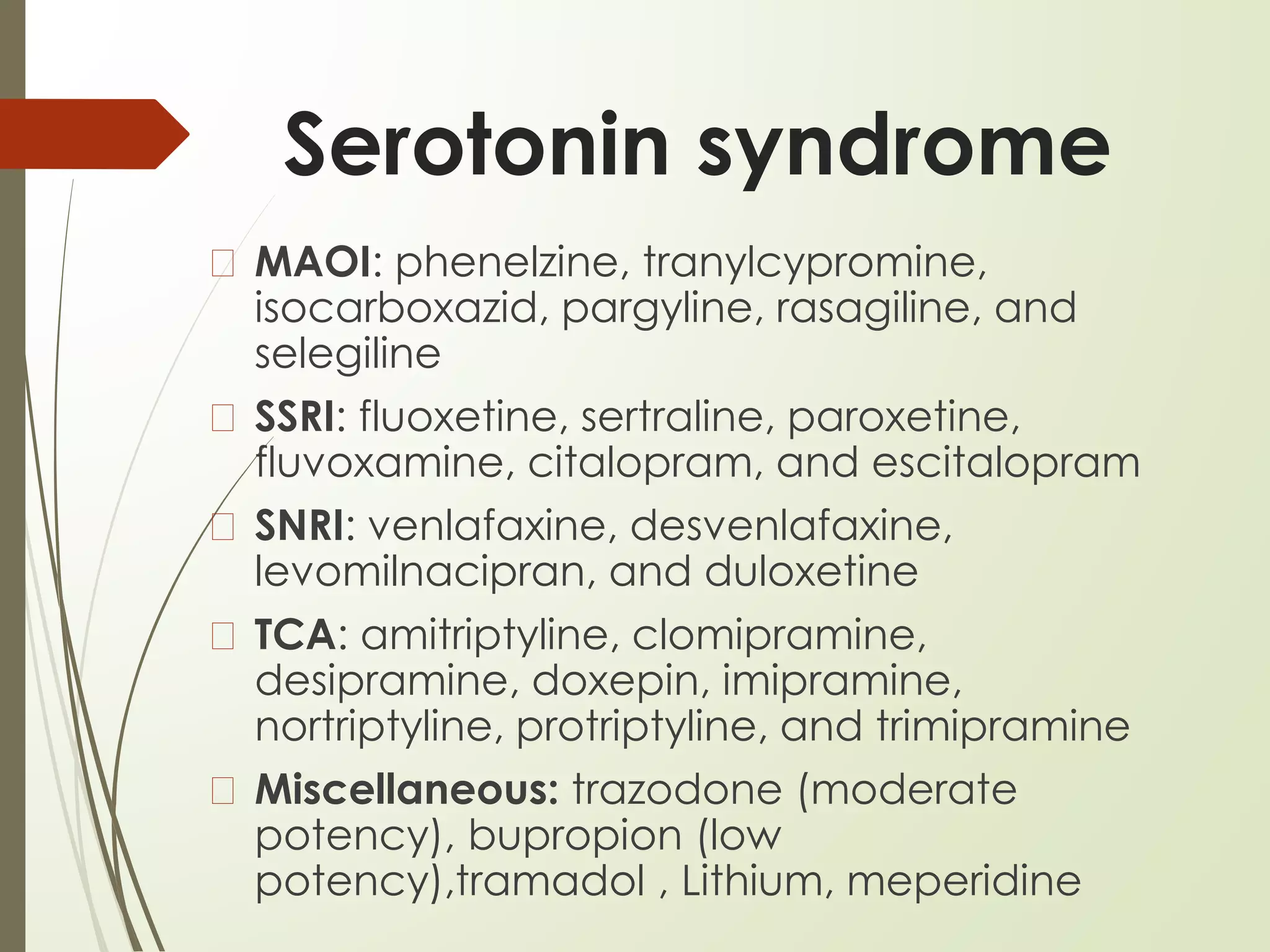
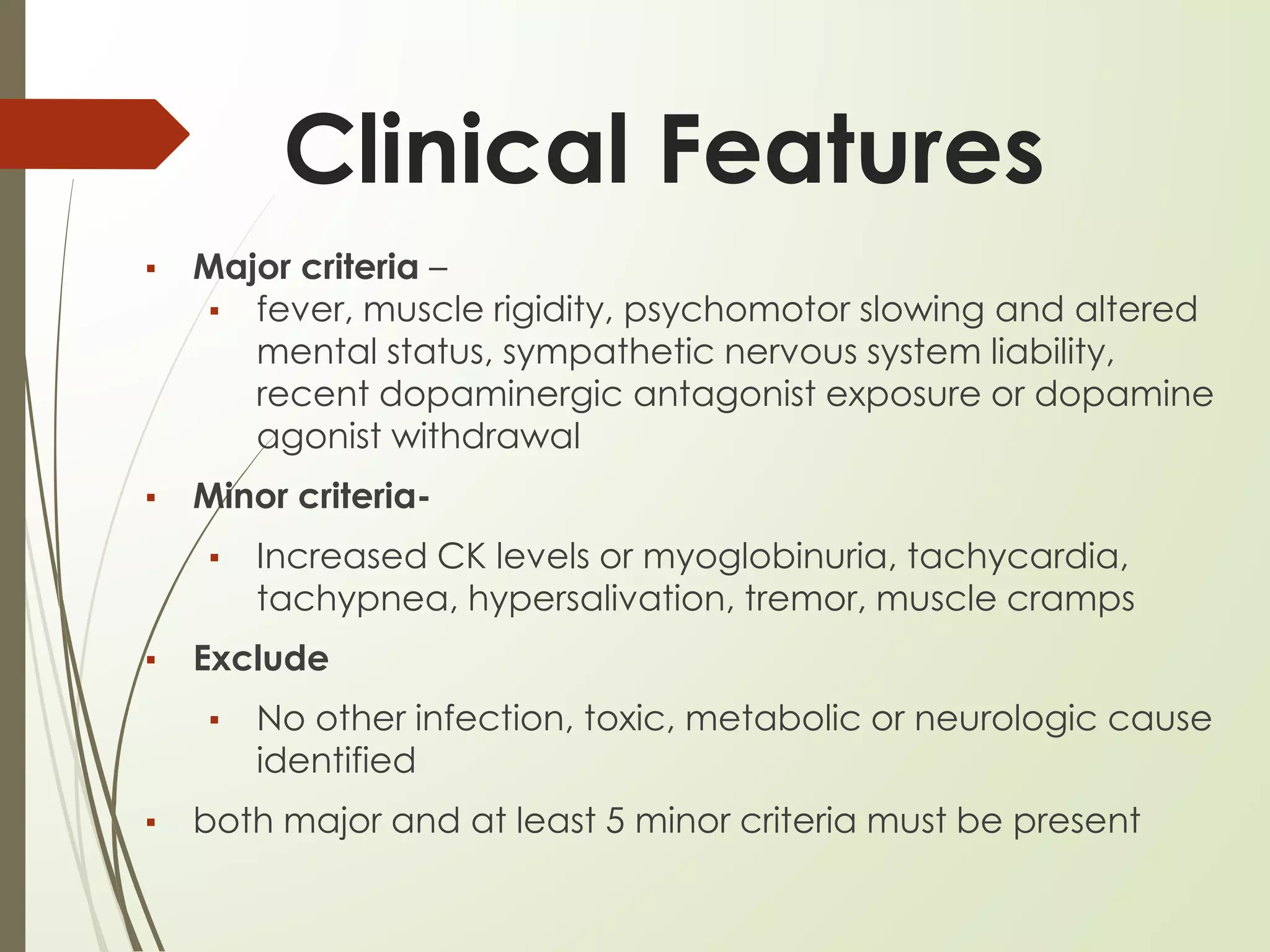
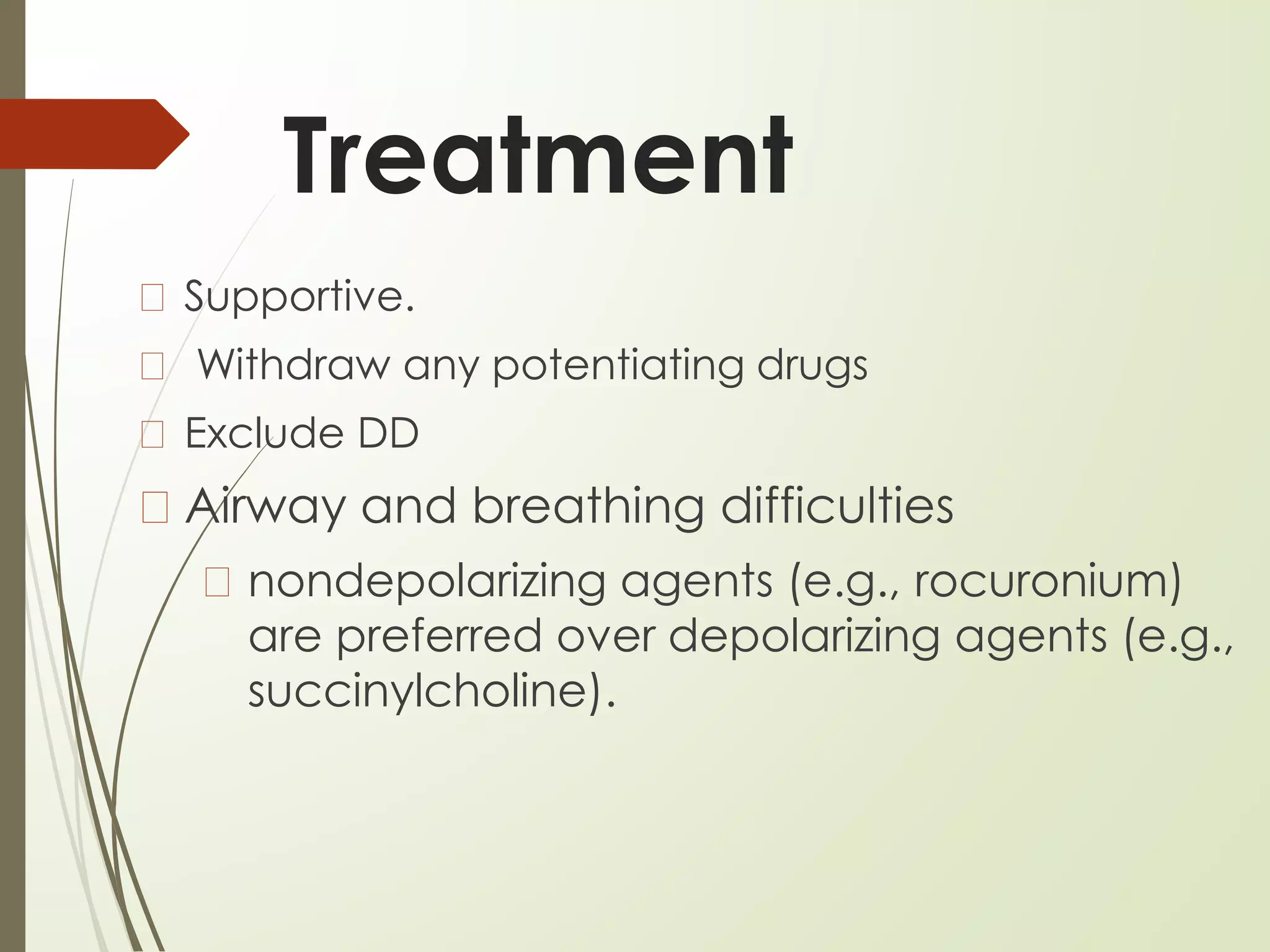
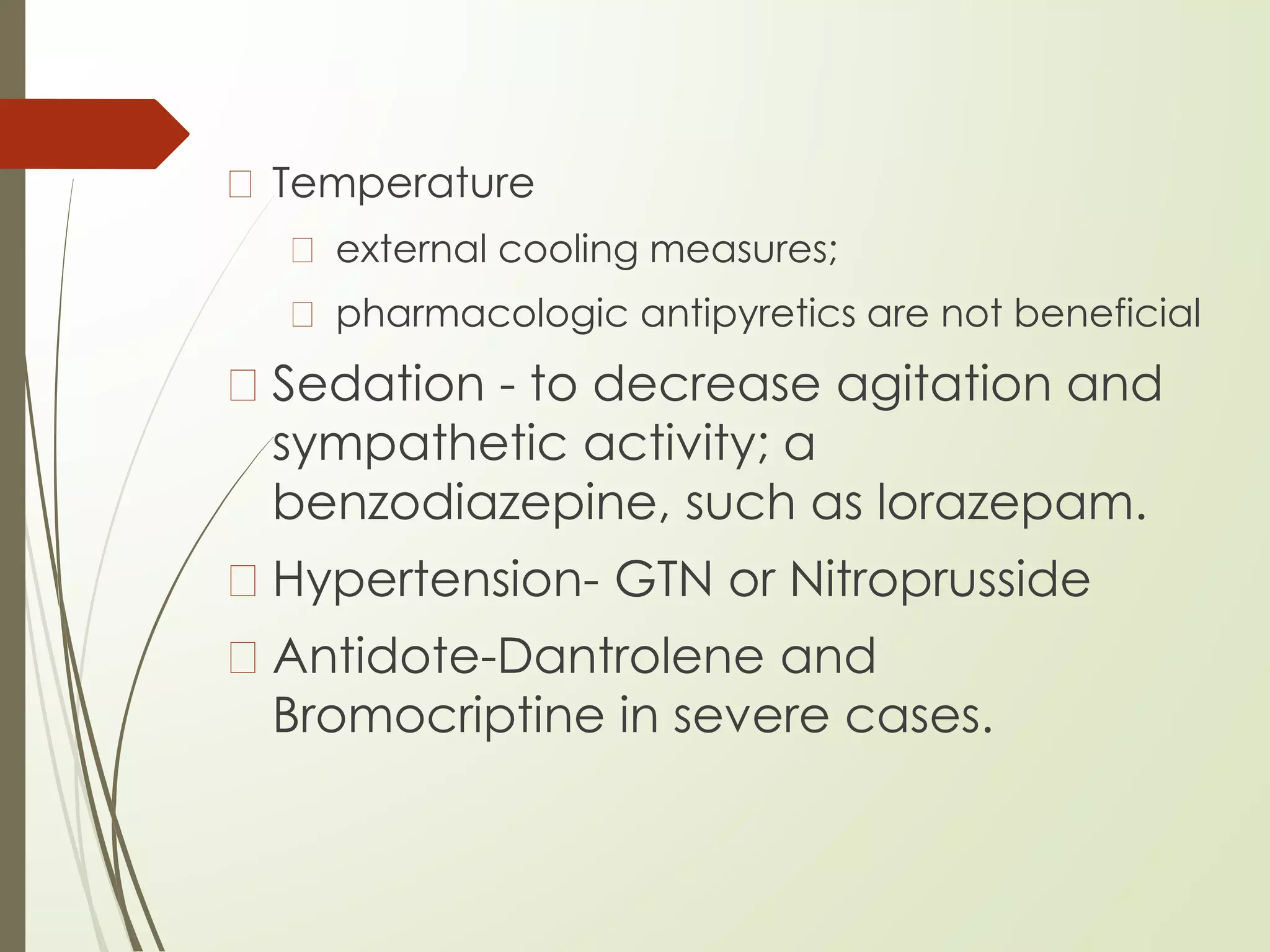
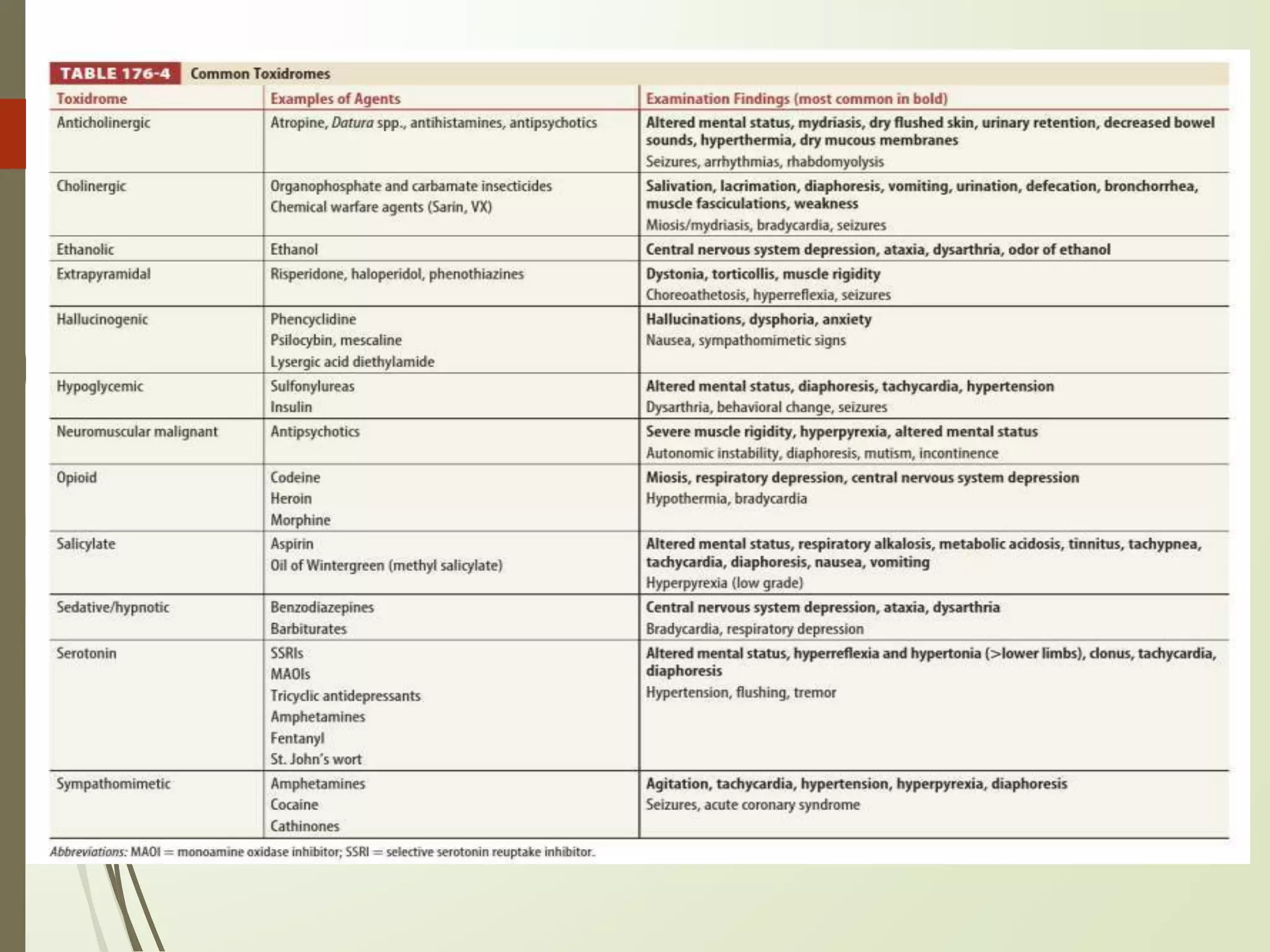
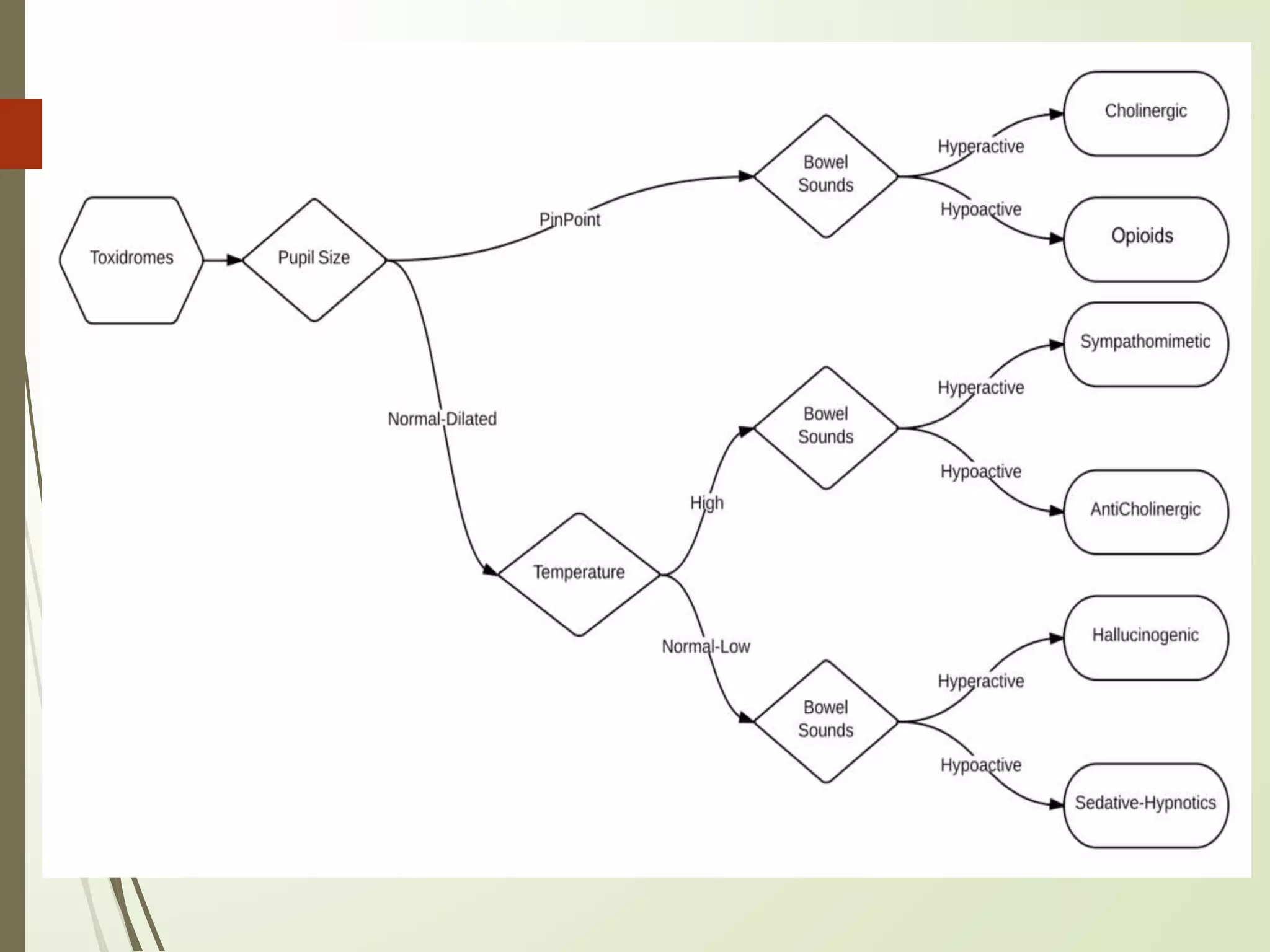
The document provides an overview of various toxidromes, categorizing toxic syndromes based on signs and symptoms, and outlines their clinical presentations and management strategies. Key toxidromes discussed include anticholinergic, cholinergic, opioid, sympathomimetic, hypno-sedative, serotonin syndrome, and neuroleptic malignant syndrome, highlighting both common causes and treatment protocols. The emphasis is placed on accurate diagnosis and effective management, utilizing patient history, physical examination, and appropriate laboratory tests.