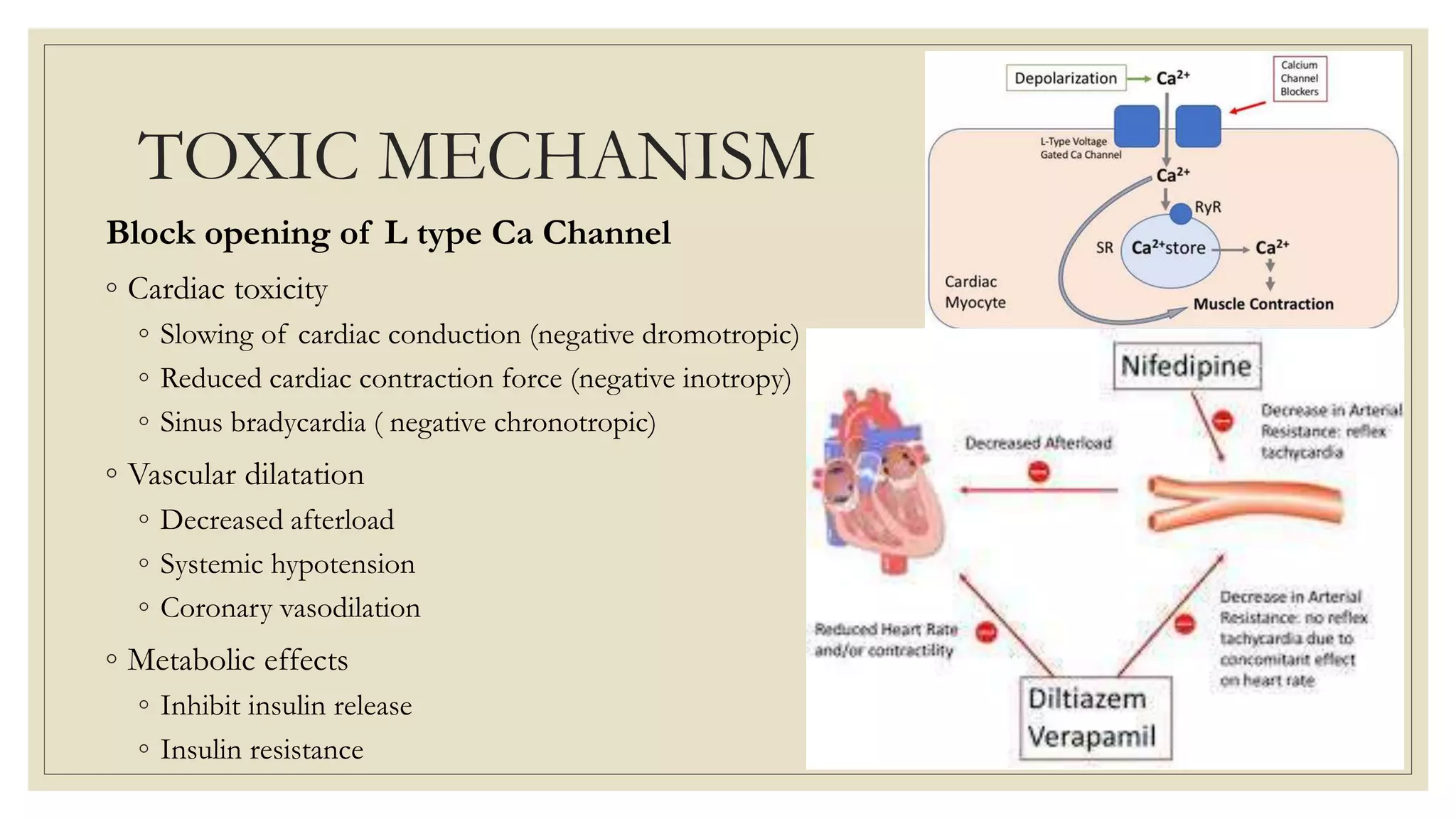
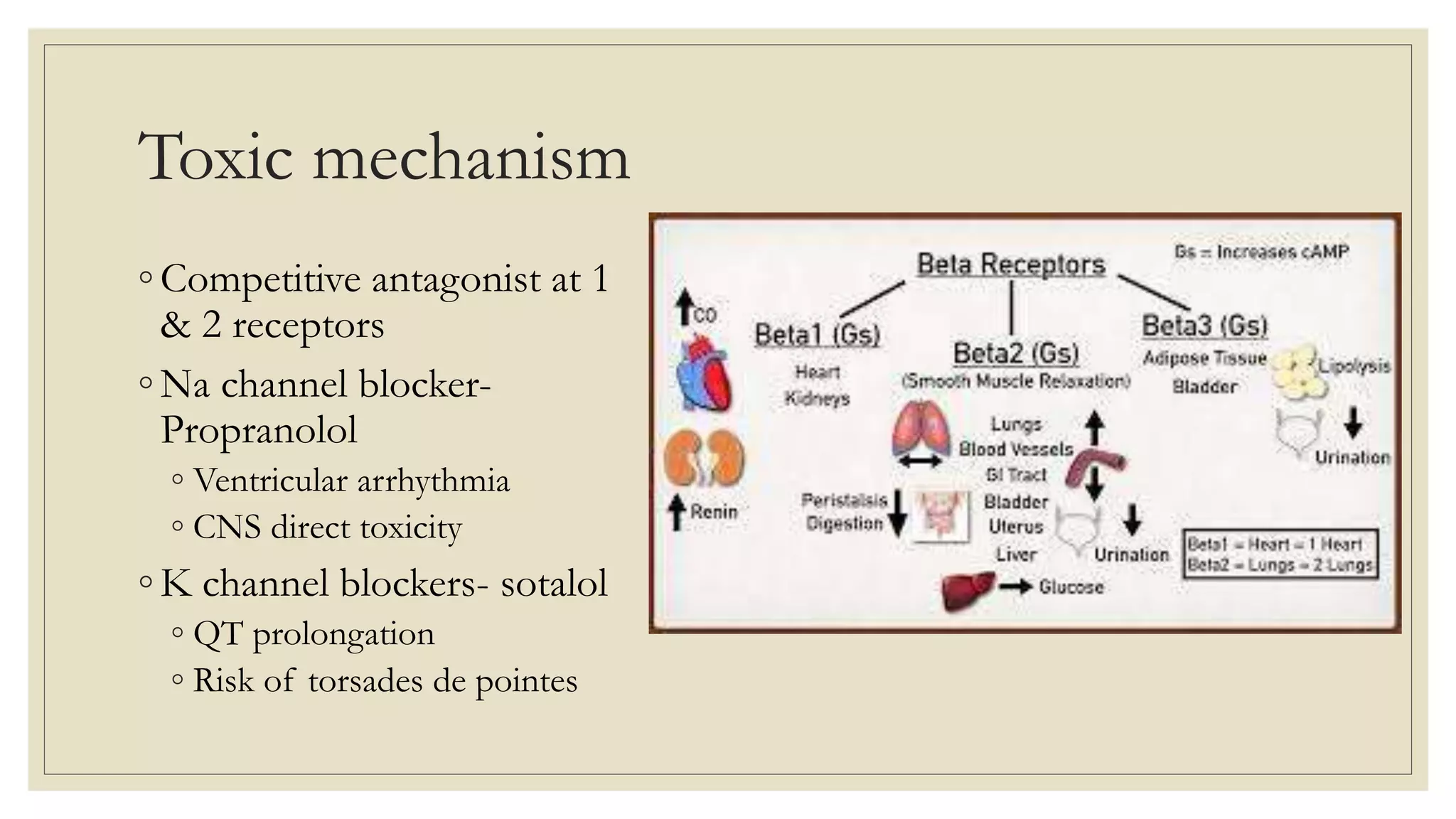
The document provides a detailed overview of calcium channel blocker (CCB) and beta-blocker poisoning, highlighting their toxic mechanisms, clinical features, and management strategies. CCB toxicity can lead to severe cardiovascular effects, while beta-blocker overdose often presents benign symptoms, with the potential for serious complications. Management includes resuscitation, supportive care, and antidotes such as high-dose insulin and glucagon, with close monitoring needed in critical care settings.