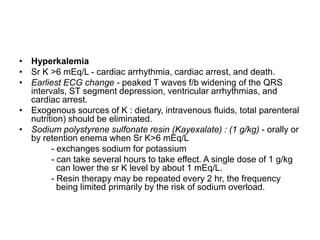
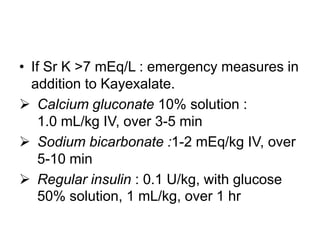
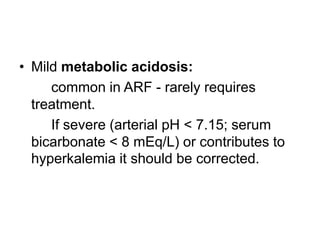
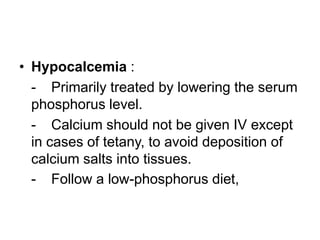
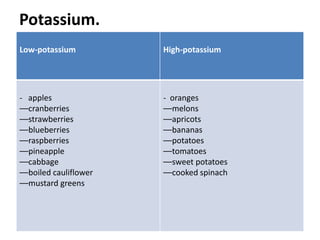
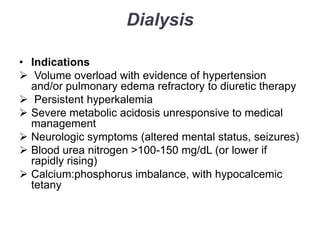
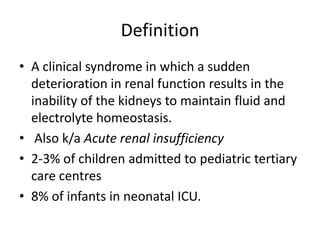
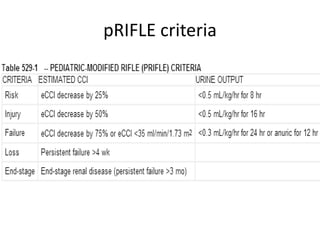
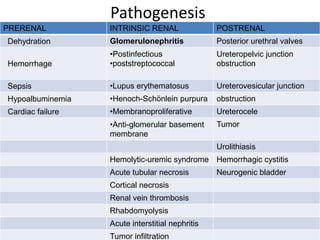
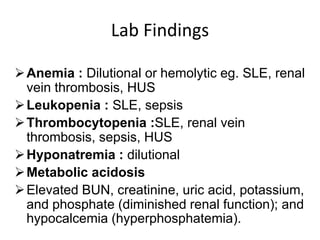
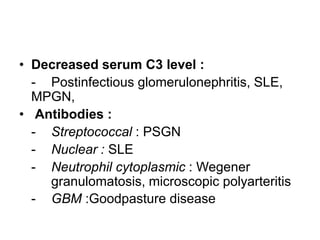
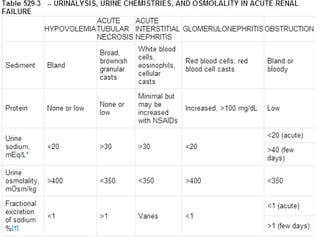
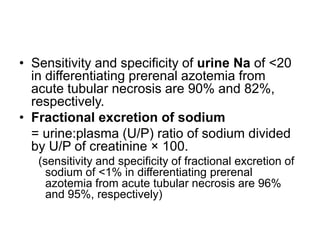
This document provides an overview of acute renal failure in children. It defines acute renal failure, discusses causes (pre-renal, intrinsic renal, post-renal), pathogenesis, laboratory findings, biomarkers, management including fluid resuscitation, diuretics, electrolyte abnormalities, nutrition, and indications for dialysis. Management is aimed at treating the underlying cause and maintaining fluid, electrolyte and acid-base balance until renal function recovers.
![• Diuretic therapy :
only after the adequate hydration.
Mannitol (0.5 g/kg) and furosemide (2-4 mg/kg) - as a
single IV dose. [Mannitol - effective in pigment
(myoglobin, hemoglobin)-induced renal failure.]
Bumetanide (0.1 mg/kg)- an alternative to furosemide.
If urine output is not improved - continuous diuretic
infusion may be considered.
Consider Dopamine (2-3 µg/kg/min) in conjunction
with diuretic therapy.
There is little evidence that diuretics or dopamine can
prevent ARF or hasten recovery.](https://image.slidesharecdn.com/acuterenalfailure-140205135305-phpapp01/85/Acute-renal-failure-in-children-14-320.jpg)