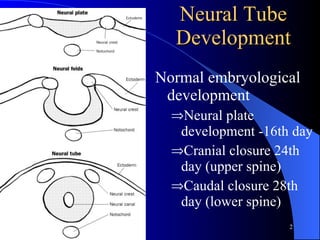
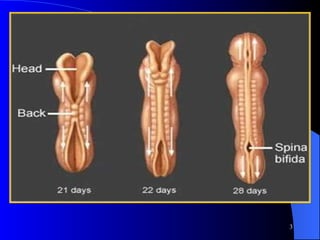
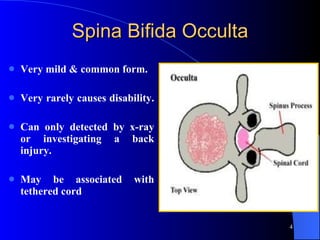
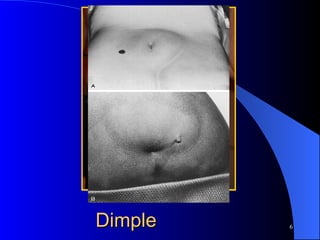
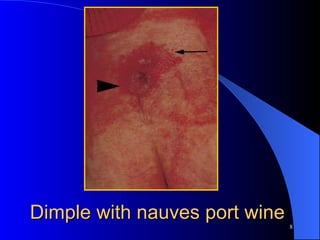
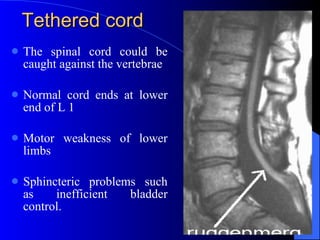
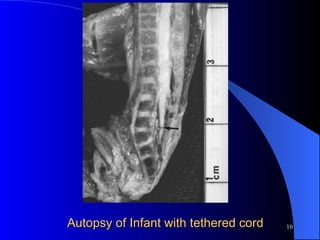
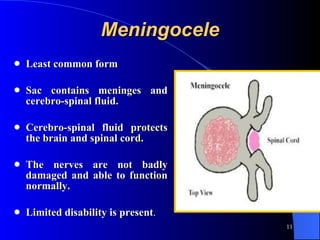
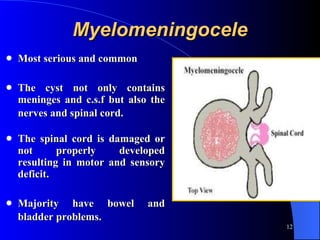
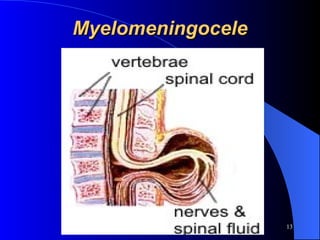
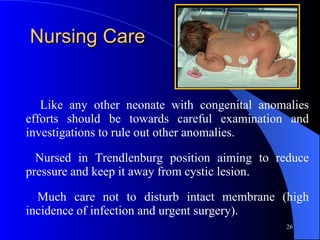
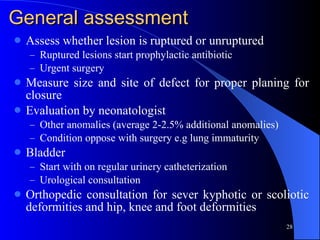
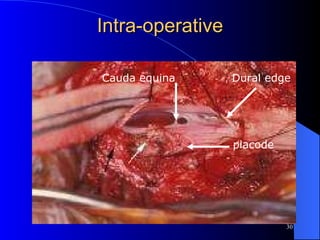
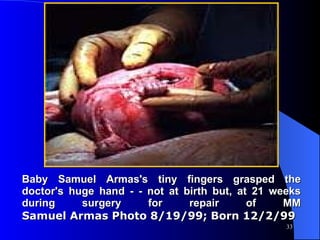
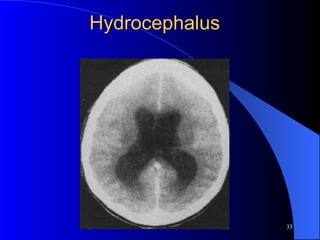
This document discusses neural tube defects (NTDs), specifically spina bifida. It describes the normal neural development process and different types of spina bifida ranging from mild to severe. Prenatal screening and diagnosis methods are outlined as well as risks factors and the importance of folic acid supplementation. Postnatal management of spina bifida newborns is also summarized.