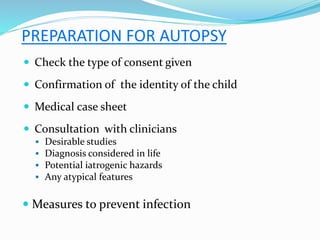
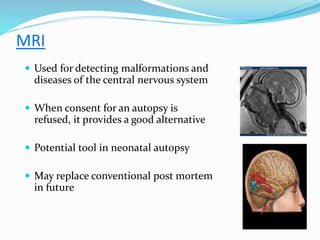
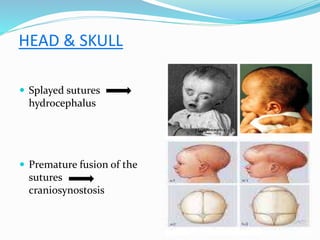
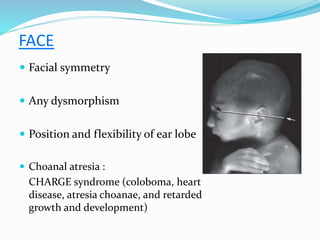
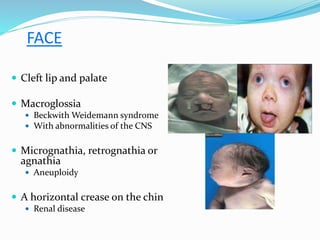
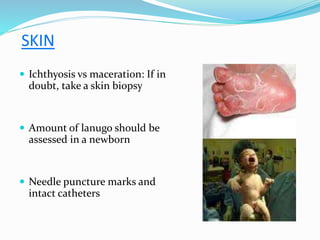
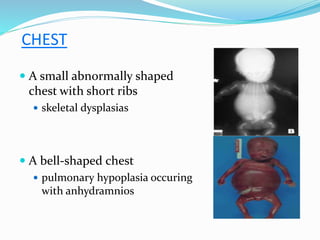
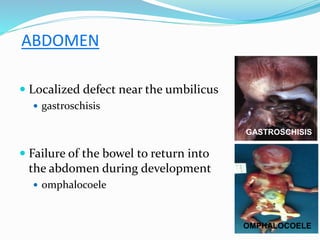
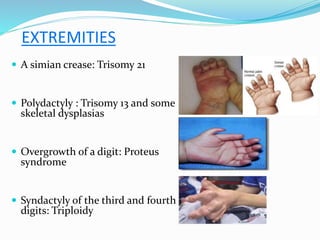
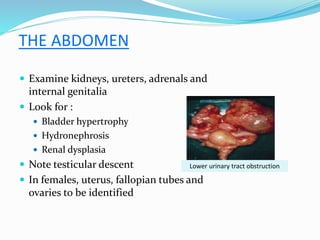
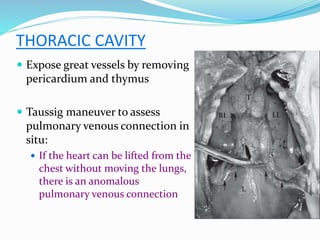
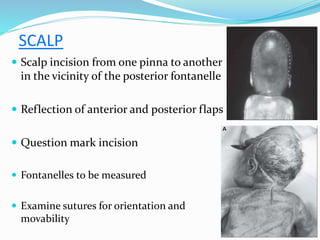
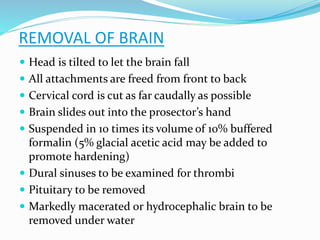
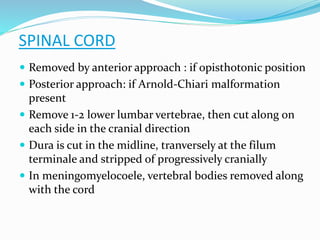
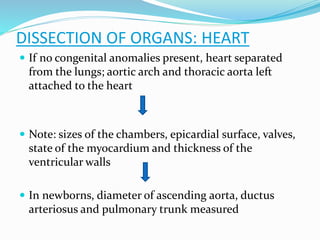
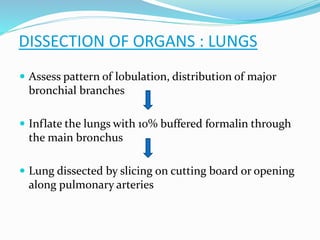
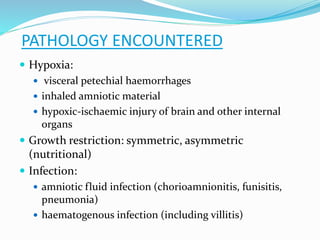
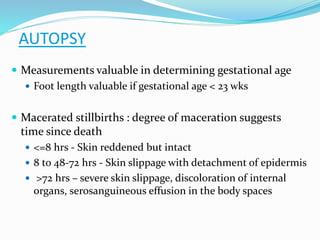
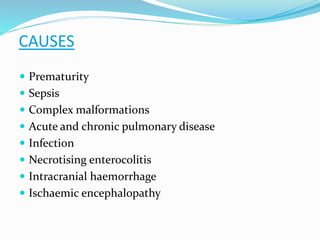
This document provides guidance on performing autopsies on pediatric cases. It discusses the purpose of pediatric autopsies which is to determine the cause of death and identify any developmental abnormalities or organ pathology. It outlines the preparation, external examination, internal examination and dissection of organs that should be conducted. Key steps include external measurements, examining features of the head, skin, chest, abdomen and extremities. The internal examination involves inspecting organs in-situ before removal and dissection of the heart, lungs, brain and other organs. Tissue sampling and imaging may also be utilized.