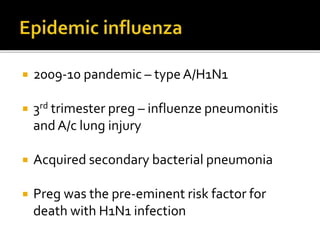
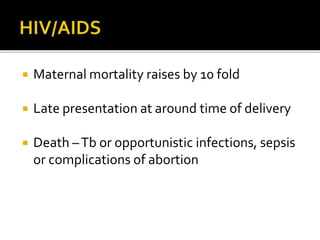
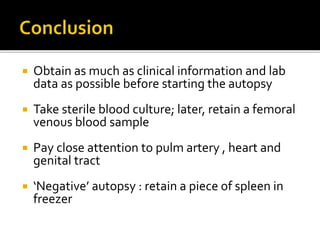
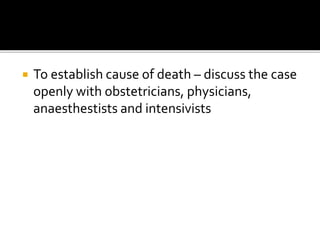
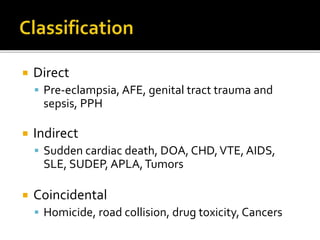
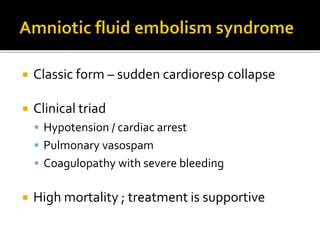
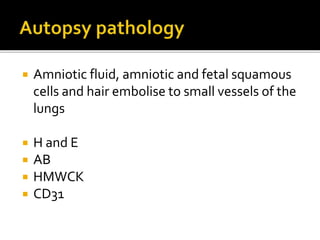
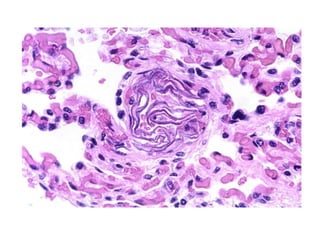
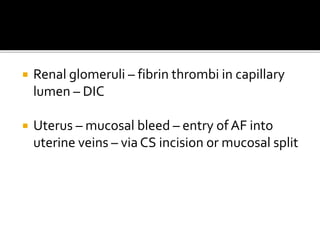
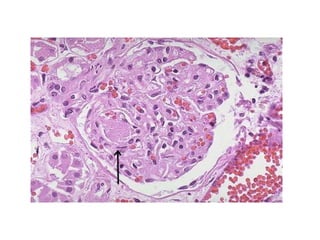
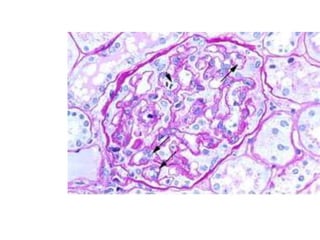
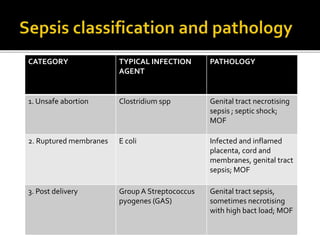
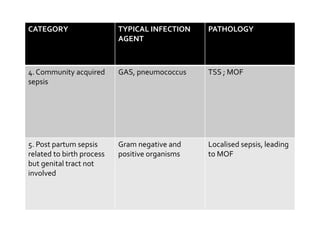
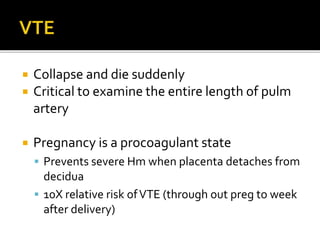
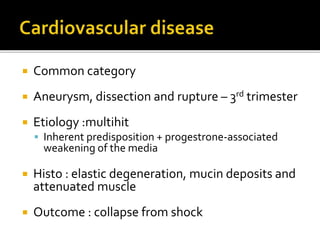
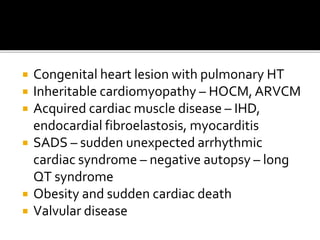
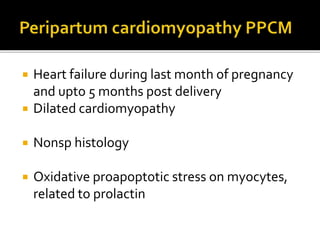
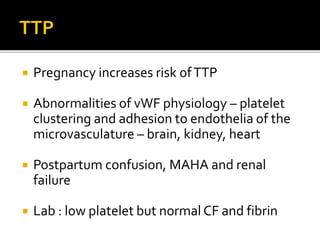
This document discusses maternal mortality and various causes of death during or after pregnancy. It covers direct causes like preeclampsia, amniotic fluid embolism, and postpartum hemorrhage. Indirect causes discussed include sudden cardiac death, venous thromboembolism, and infections. The document provides details on evaluating different conditions pathological findings. It stresses the importance of a thorough autopsy including samples, cultures, and examination of key organs to determine the cause of maternal death.

![ Preg – relative immunodep state [CMI ]
Viral infection ( HS , hepatitis , influenza )
Listeriosis
Tb](https://image.slidesharecdn.com/thematernaldeathautopsy-150329085817-conversion-gate01/85/The-maternal-death-autopsy-33-320.jpg)