This document provides instructions for performing an autopsy on the brain. Key steps include:
1. Making incisions in the scalp and sawing the skull to remove the skull cap.
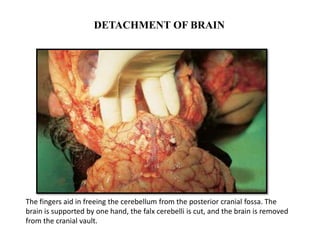
2. Detaching the brain by cutting cranial nerves and blood vessels at the base and severing the spinal cord.
3. Weighing and examining the fresh brain before fixation.
4. Immersing the brain in formalin for 10-14 days to fix the tissue.
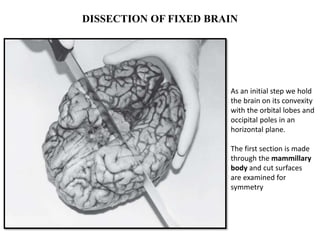
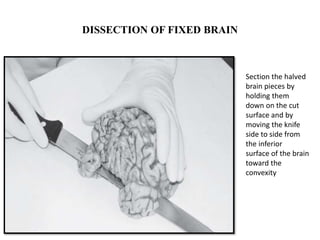
5. Dissecting the fixed brain by making coronal and horizontal cuts to examine the structures.
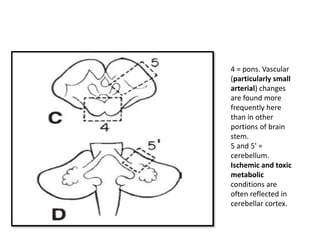
6. Selecting tissue blocks for microscopic examination, including areas like the frontal lobes, basal ganglia, hippocampus, pons