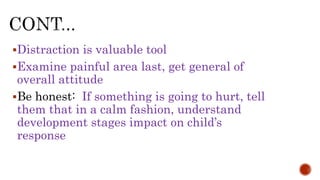
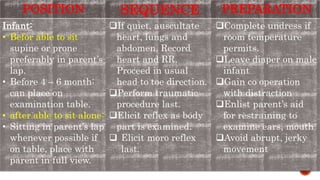
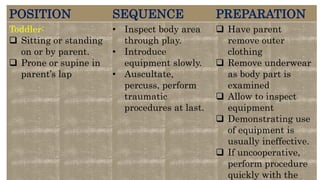
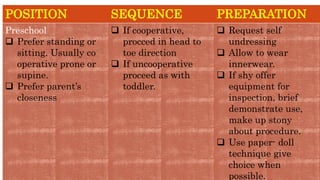
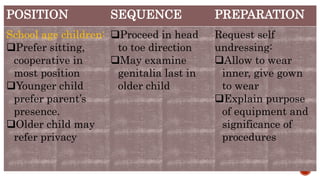
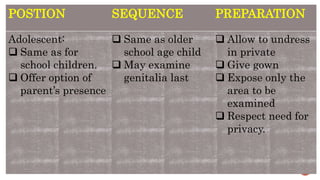
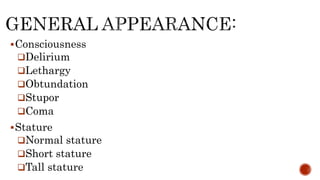
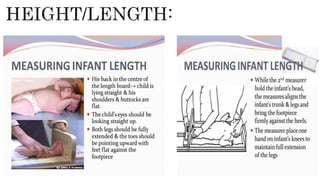
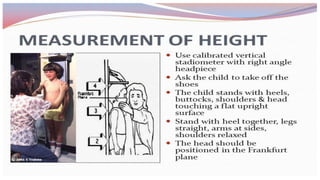
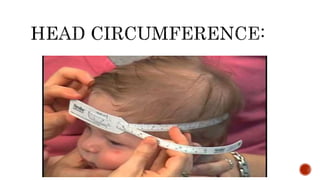
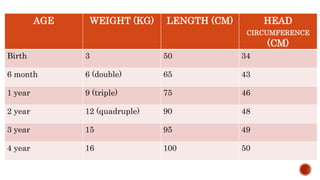
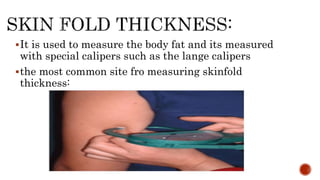
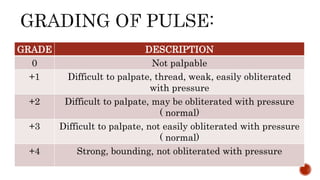
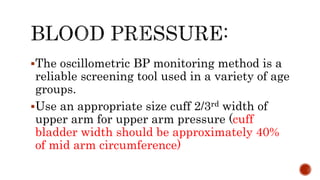
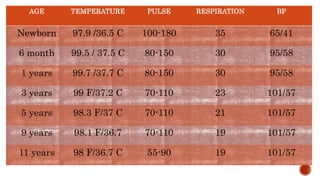
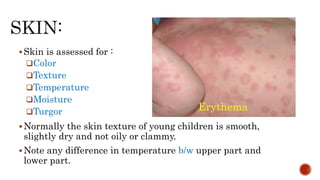
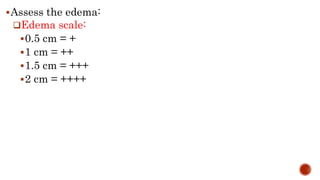
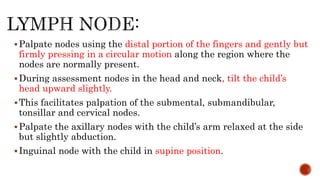
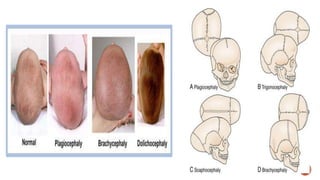
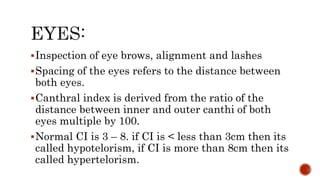
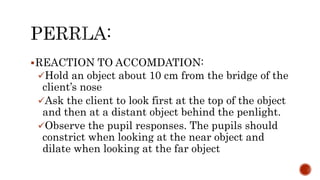
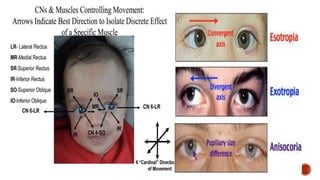
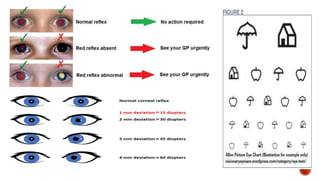
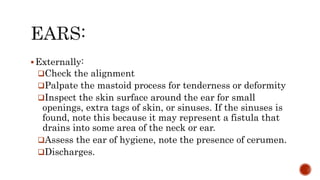
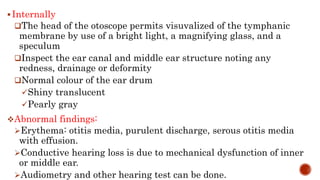
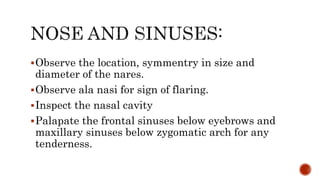
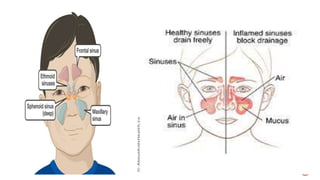
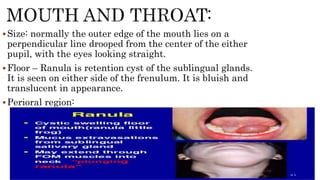
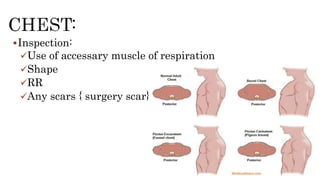
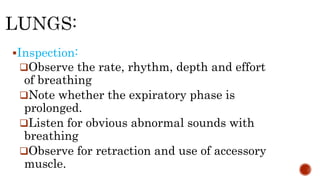
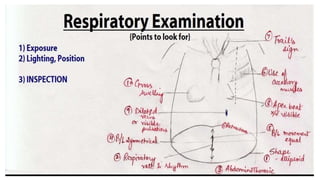
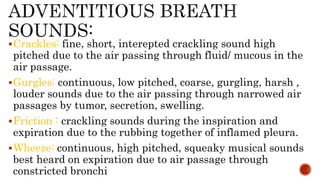
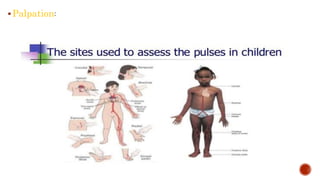
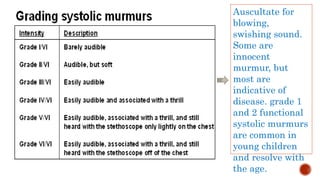
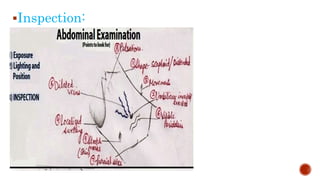
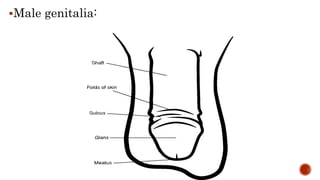
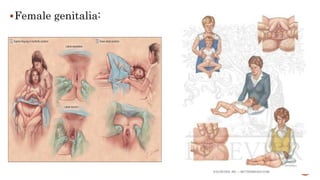
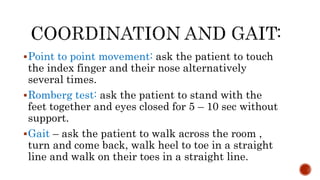
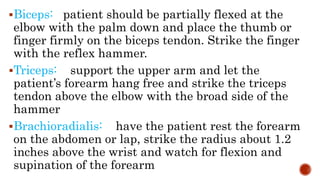
The document provides guidance on performing a physical examination on children of different ages. It discusses the key aspects of examination including positioning the child, examination sequence, and preparation. For each age group (infant, toddler, preschooler, school-aged, adolescent), it recommends an ideal position, examination sequence, and tips for preparation to make the child comfortable and cooperative. The document also outlines guidelines for assessing various vital signs and performing a head-to-toe examination, with notes on normal values and signs of concern for different body systems.