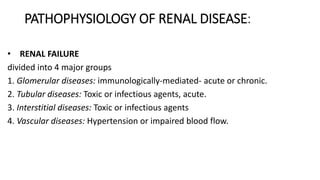
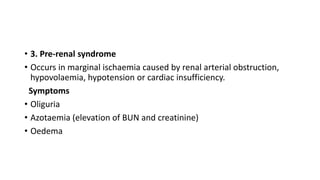
1. Renal failure can be acute or chronic and is classified based on the underlying cause and pathology. Acute renal failure (ARF) is characterized by a rapid decline in renal function and accumulation of waste products in the blood. Common causes of ARF include decreased blood flow to the kidneys, direct kidney damage, or urinary tract obstruction.
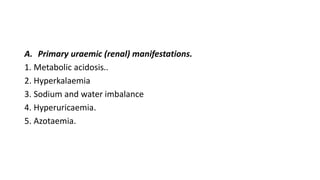
2. Chronic renal failure (CRF) is an irreversible deterioration of renal function that develops slowly over time. It can be caused by diseases affecting the glomeruli or tubulointerstitial tissues. CRF results in fluid and electrolyte imbalances as well as metabolic abnormalities that manifest as uraemic symptoms.
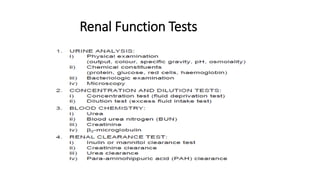
3. Laboratory findings in renal