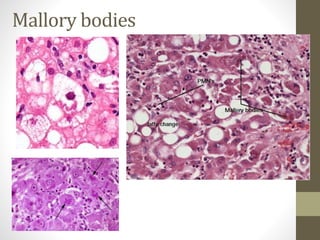
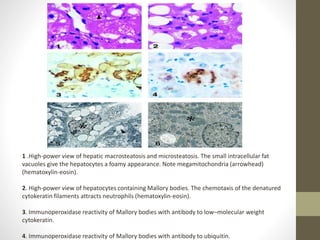
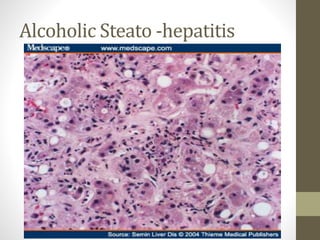
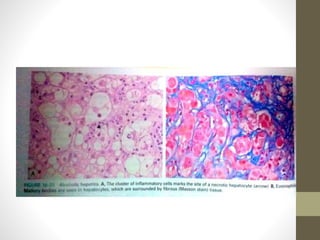
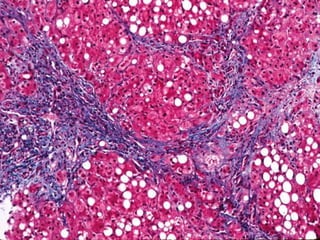
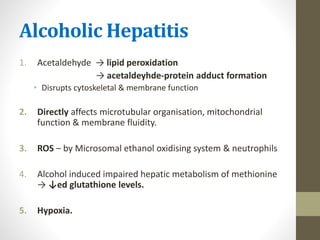
1. Alcoholic hepatitis is characterized by hepatocyte swelling and necrosis, Mallory bodies, neutrophil infiltration and fibrosis. Mallory bodies are tangled skeins of cytokeratin intermediate filaments that appear as eosinophilic cytoplasmic inclusions.
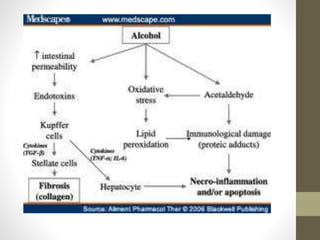
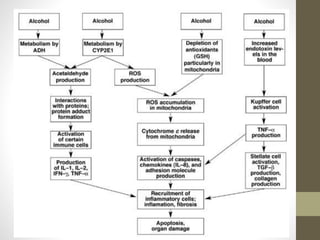
2. Alcohol metabolism leads to lipid peroxidation, acetaldehyde-protein adduct formation and reactive oxygen species production, impairing hepatic function. Cytokines such as TNF are the main mediators of alcoholic liver injury.
3. Clinical features of alcoholic hepatitis include malaise, anorexia, tender hepatomegaly, fever, hyperbilirubinemia and elevated liver enzymes. Later stages develop complications like ascites, variceal bleeding and