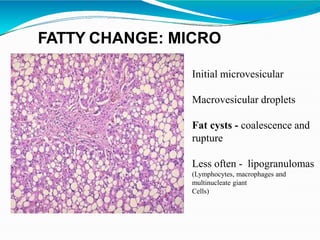
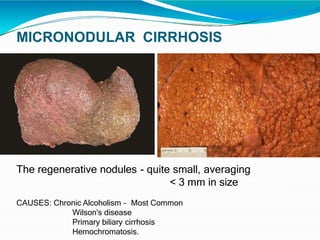
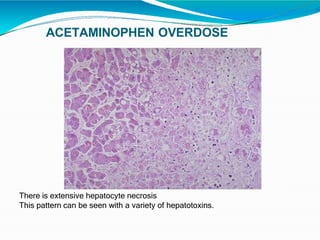
This document provides an overview of liver pathology, covering topics such as normal liver anatomy and histology, biopsy techniques, viral hepatitis, cirrhosis, tumors, and other disorders. It begins with a basic introduction and table of contents, then discusses the liver's structure and function at both the gross and microscopic level. Specific pathological conditions are described in detail, with information on etiology, gross and microscopic appearance, important histological stains, and differential diagnosis when relevant. These include fatty liver disease, viral hepatitis, cirrhosis, vascular and pigmentary disorders, as well as benign and malignant epithelial and mesenchymal tumors.