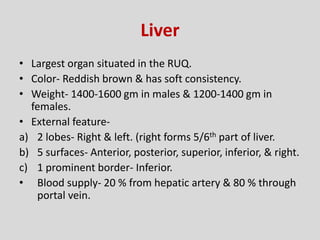
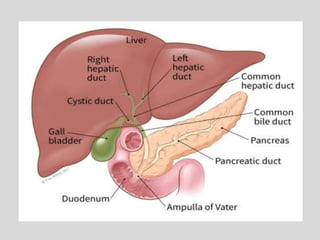
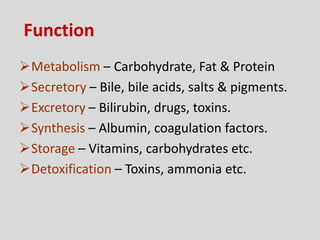
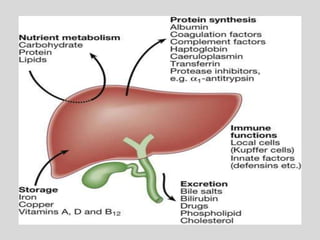
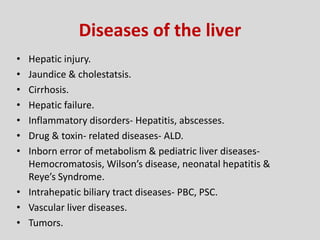
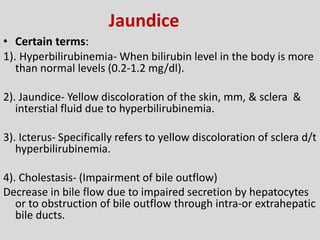
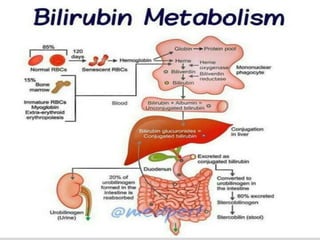
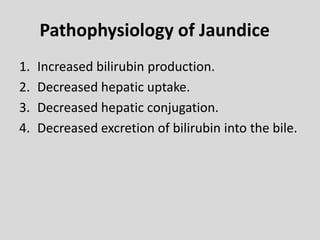
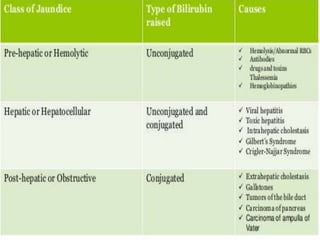
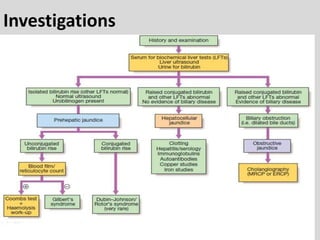
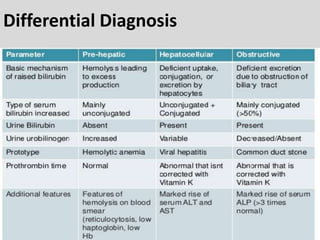
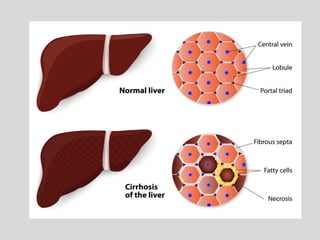
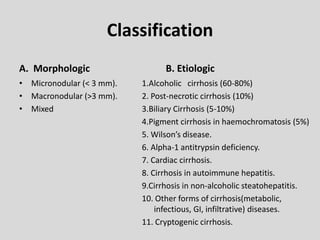
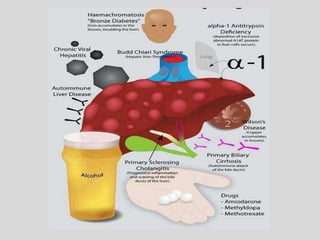
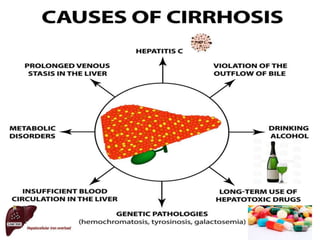
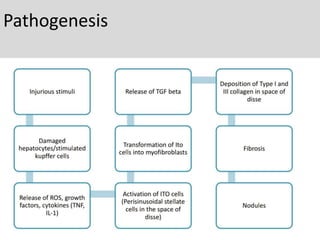
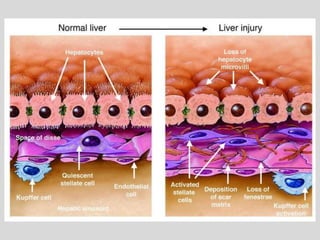
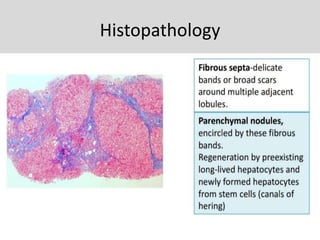
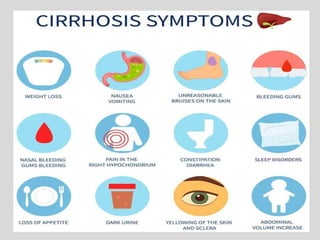
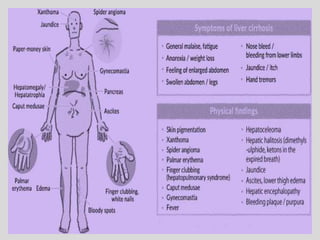
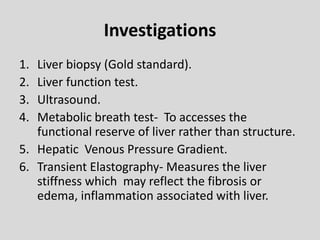
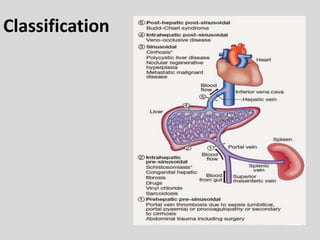
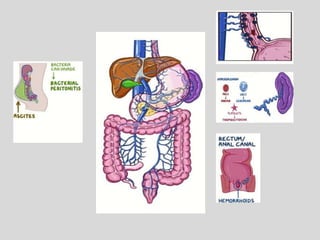
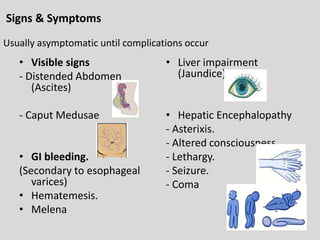
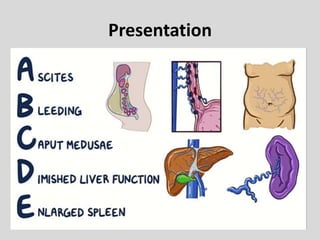
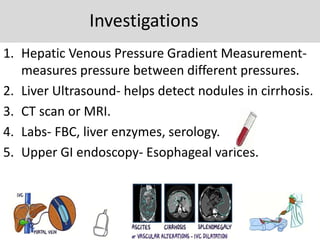
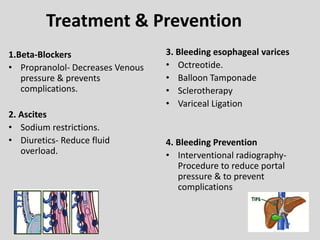
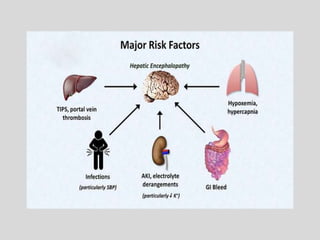
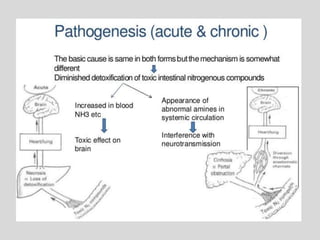
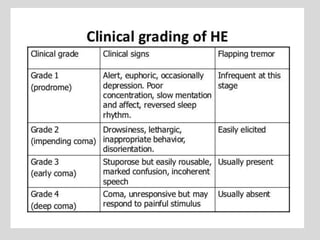
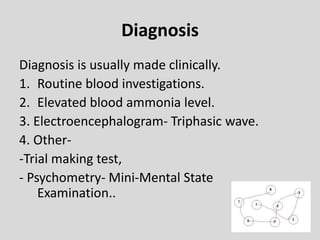
This document provides information on liver pathology and disease. It begins with the anatomy and functions of the liver. It then discusses various liver diseases including hepatic injury, cirrhosis, hepatitis, and tumors. It also provides in-depth descriptions of jaundice, portal hypertension, and hepatic encephalopathy - discussing their causes, signs/symptoms, investigations, and treatments. The document is an informative overview of liver conditions and diseases.