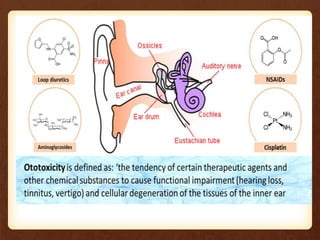
The lecture on ototoxicity outlines its definition, causes, assessment, and management strategies. Ototoxicity, or ear poisoning, can lead to hearing loss due to various medications, with common ototoxic drugs including certain antibiotics and chemotherapy agents. Management focuses on monitoring medication effects, rehabilitating function, and utilizing hearing aids or cochlear implants as necessary.