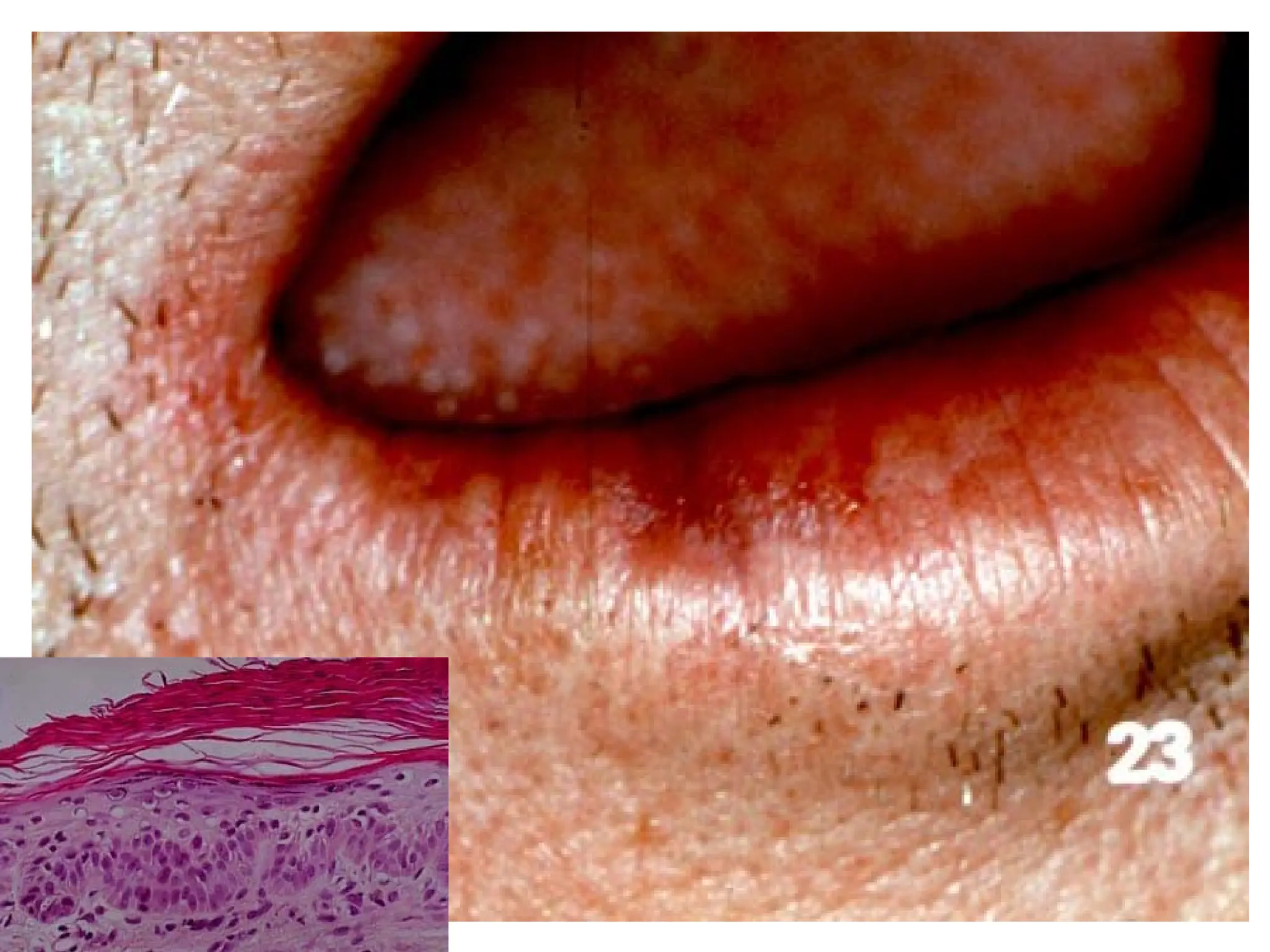
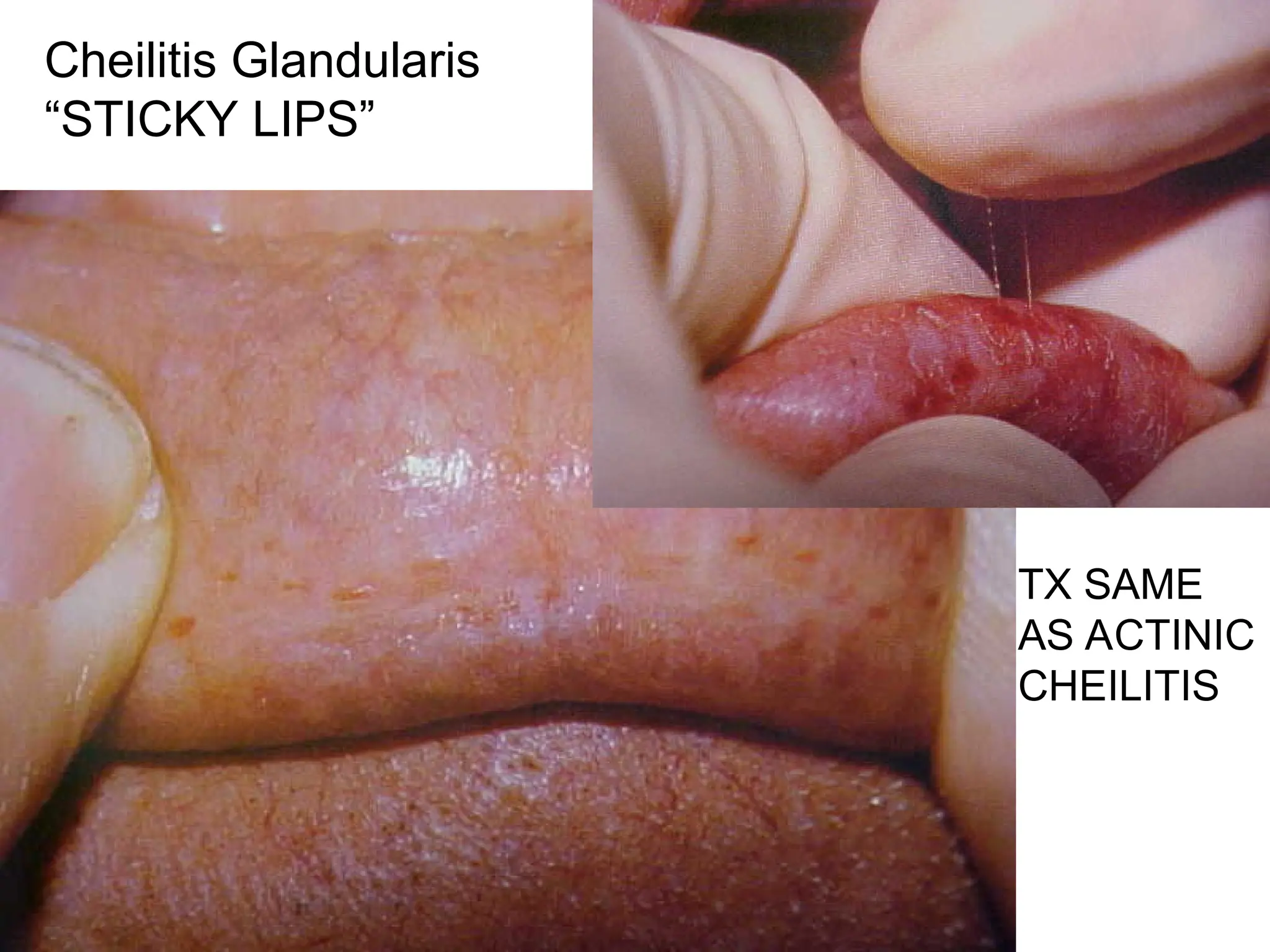
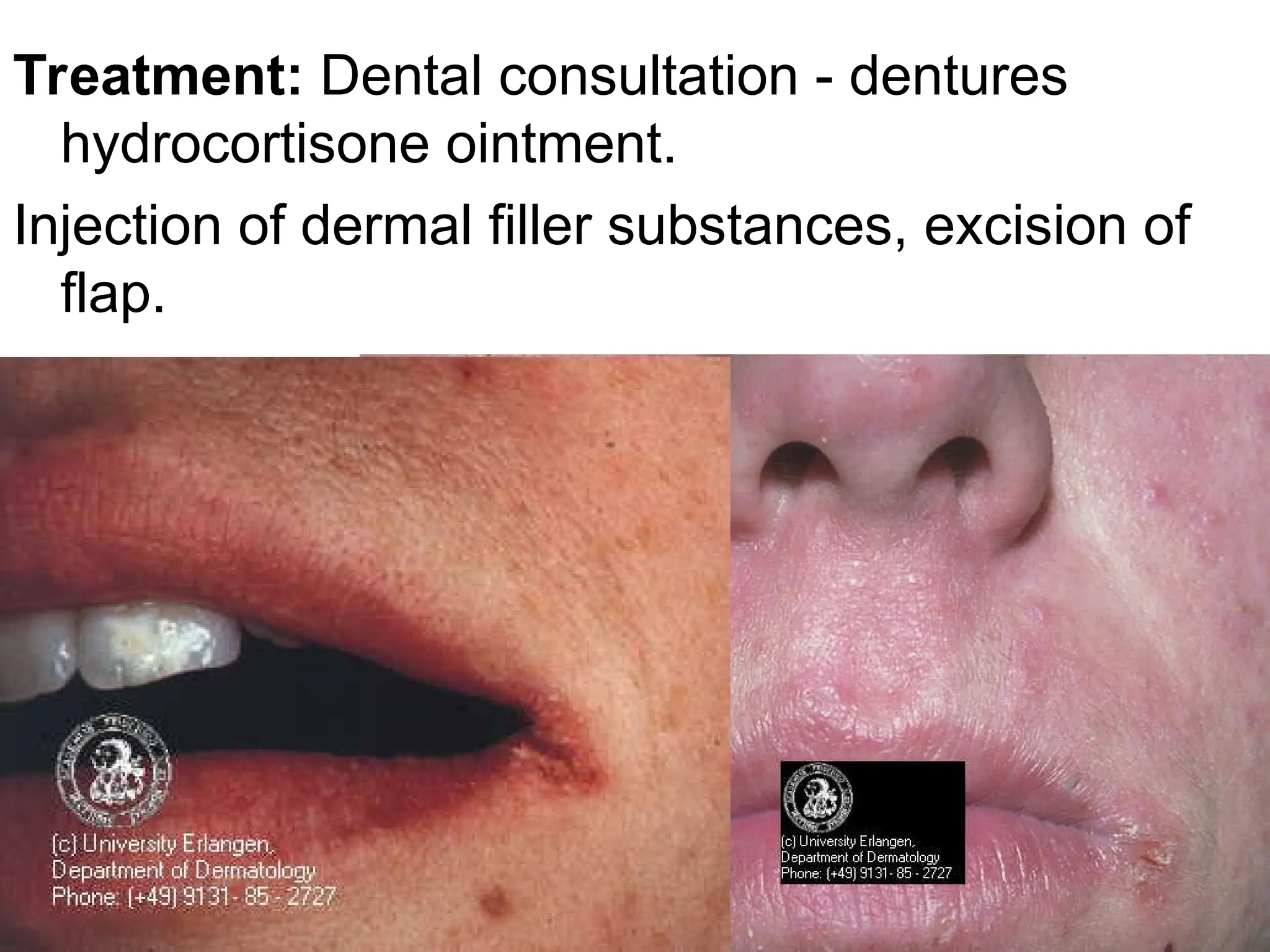
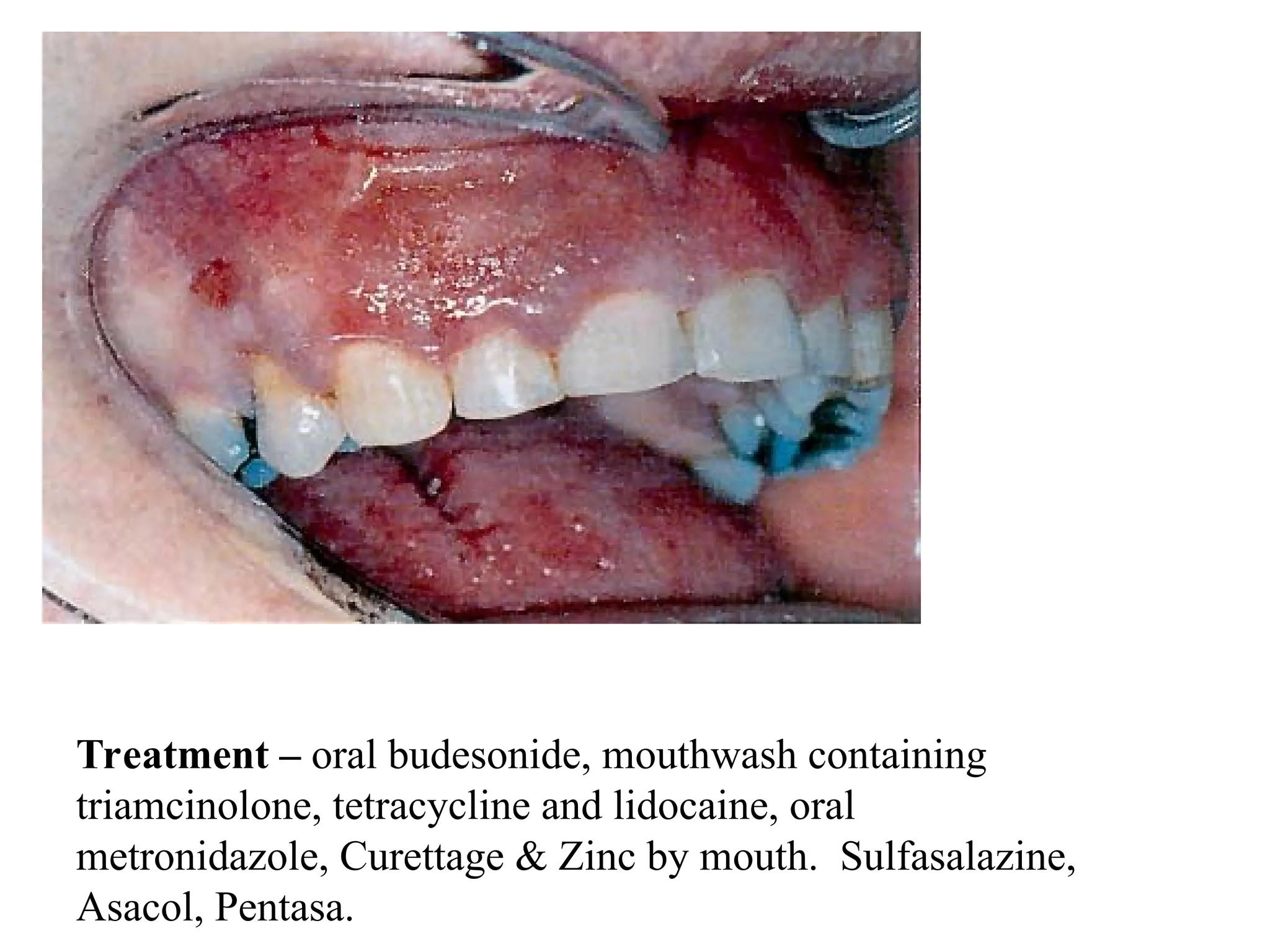
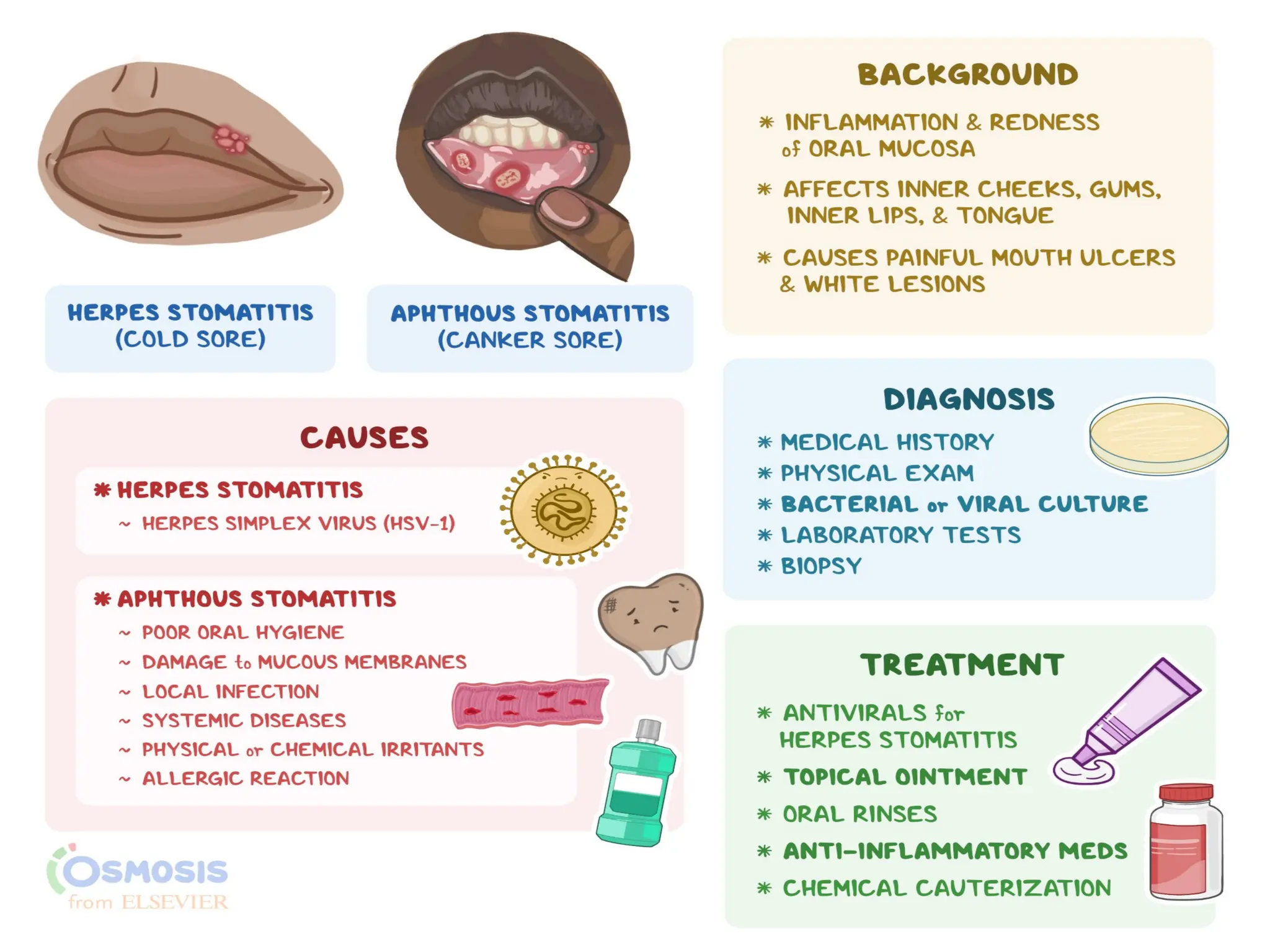
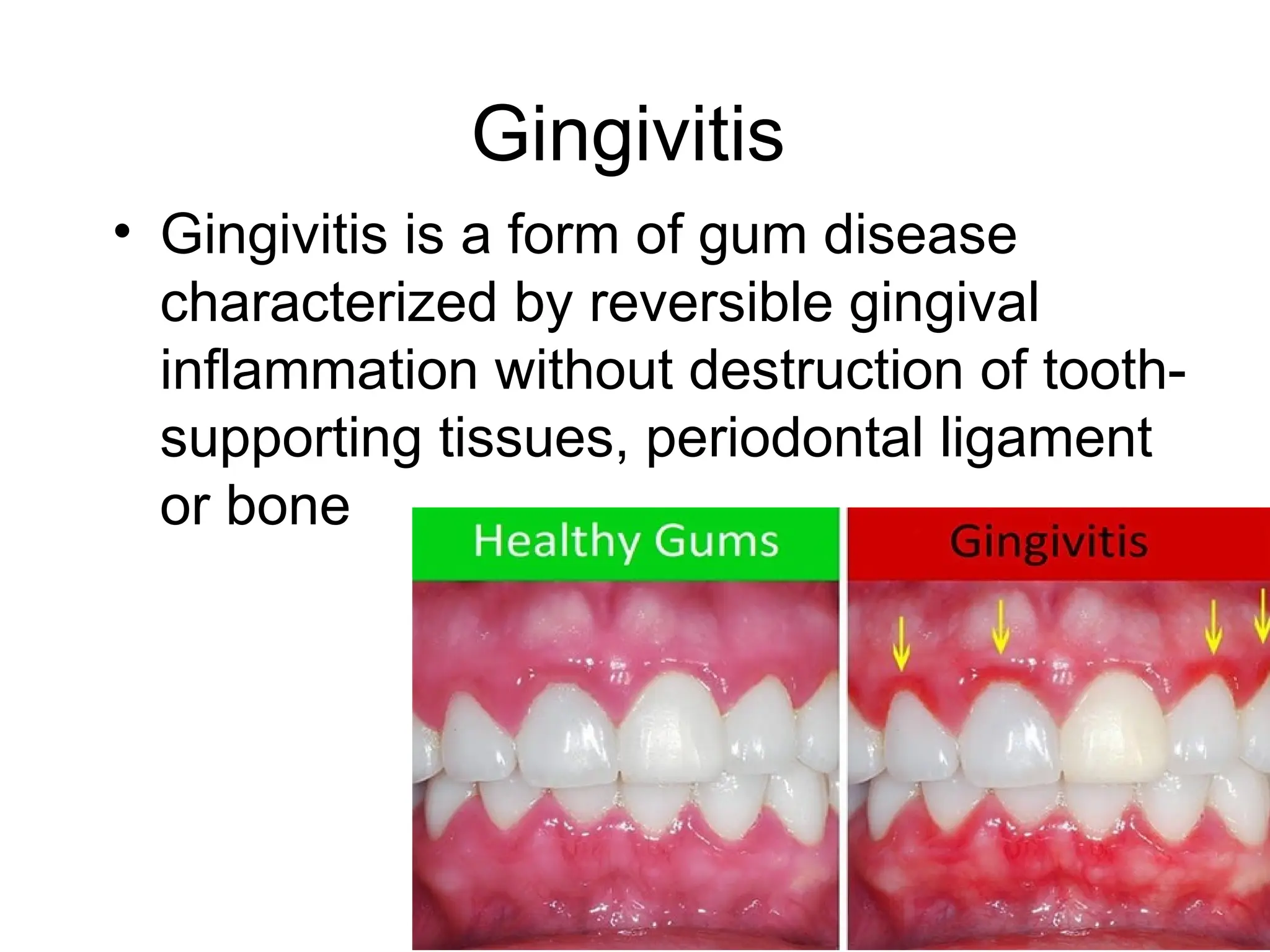
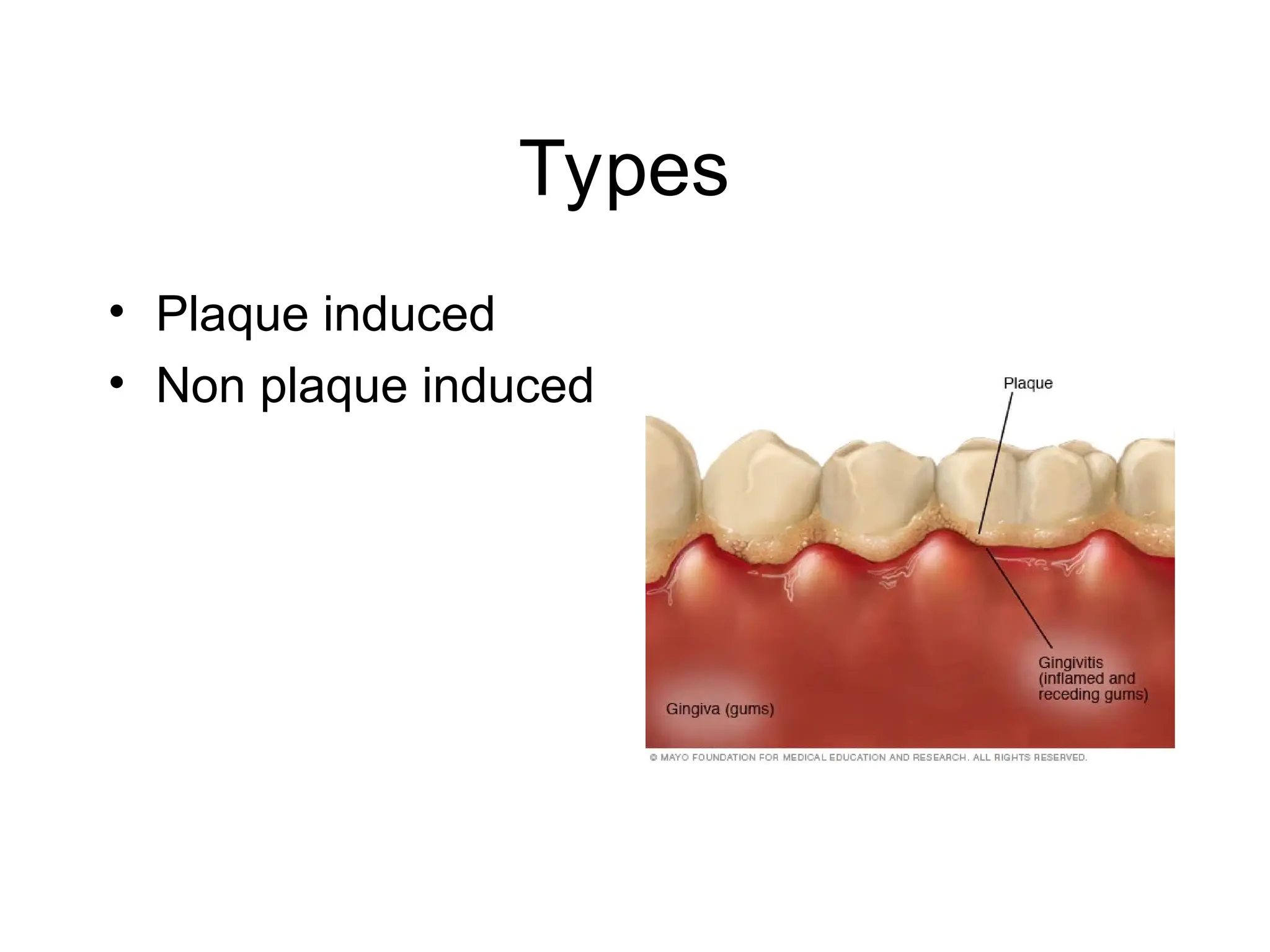
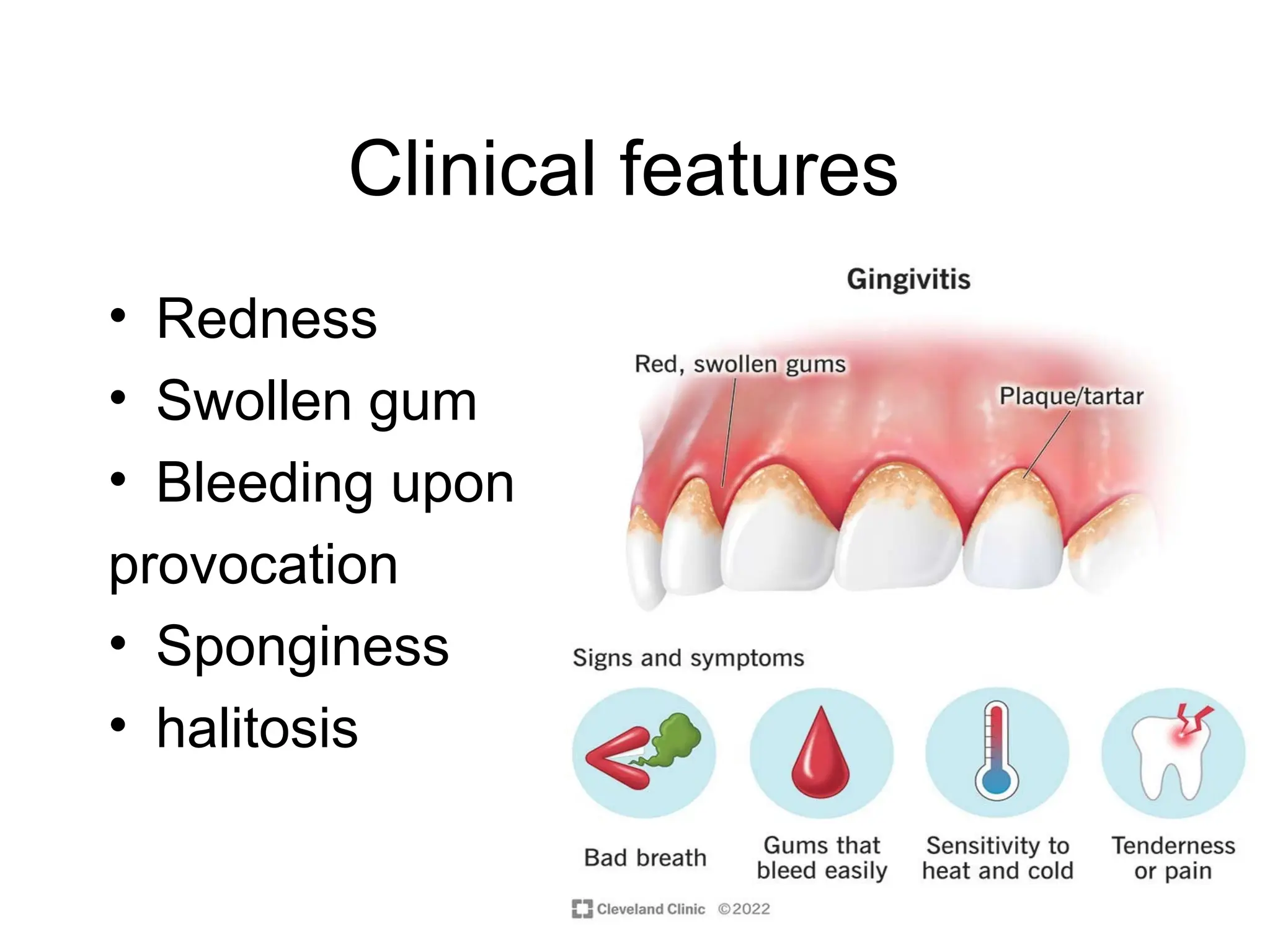
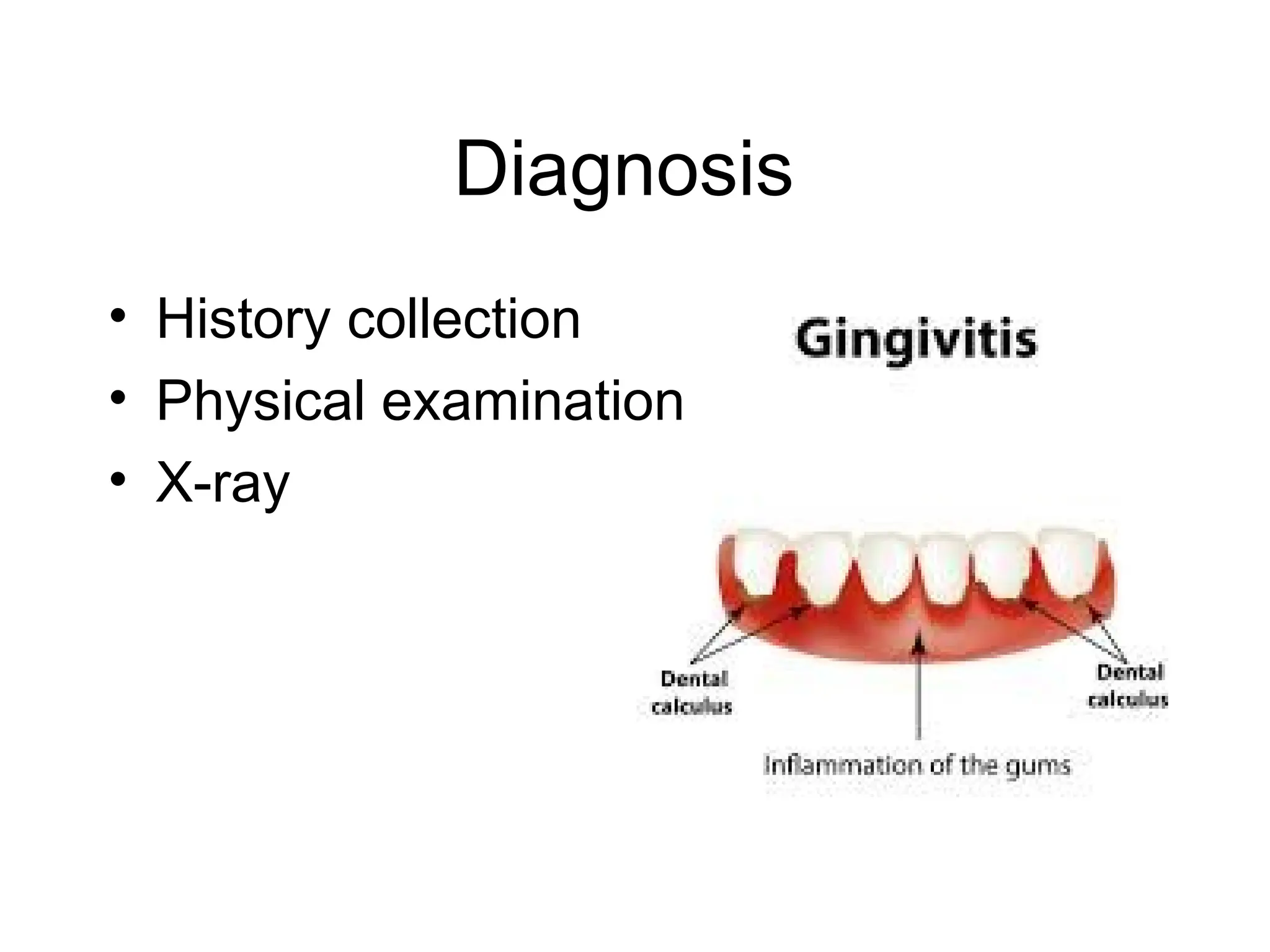
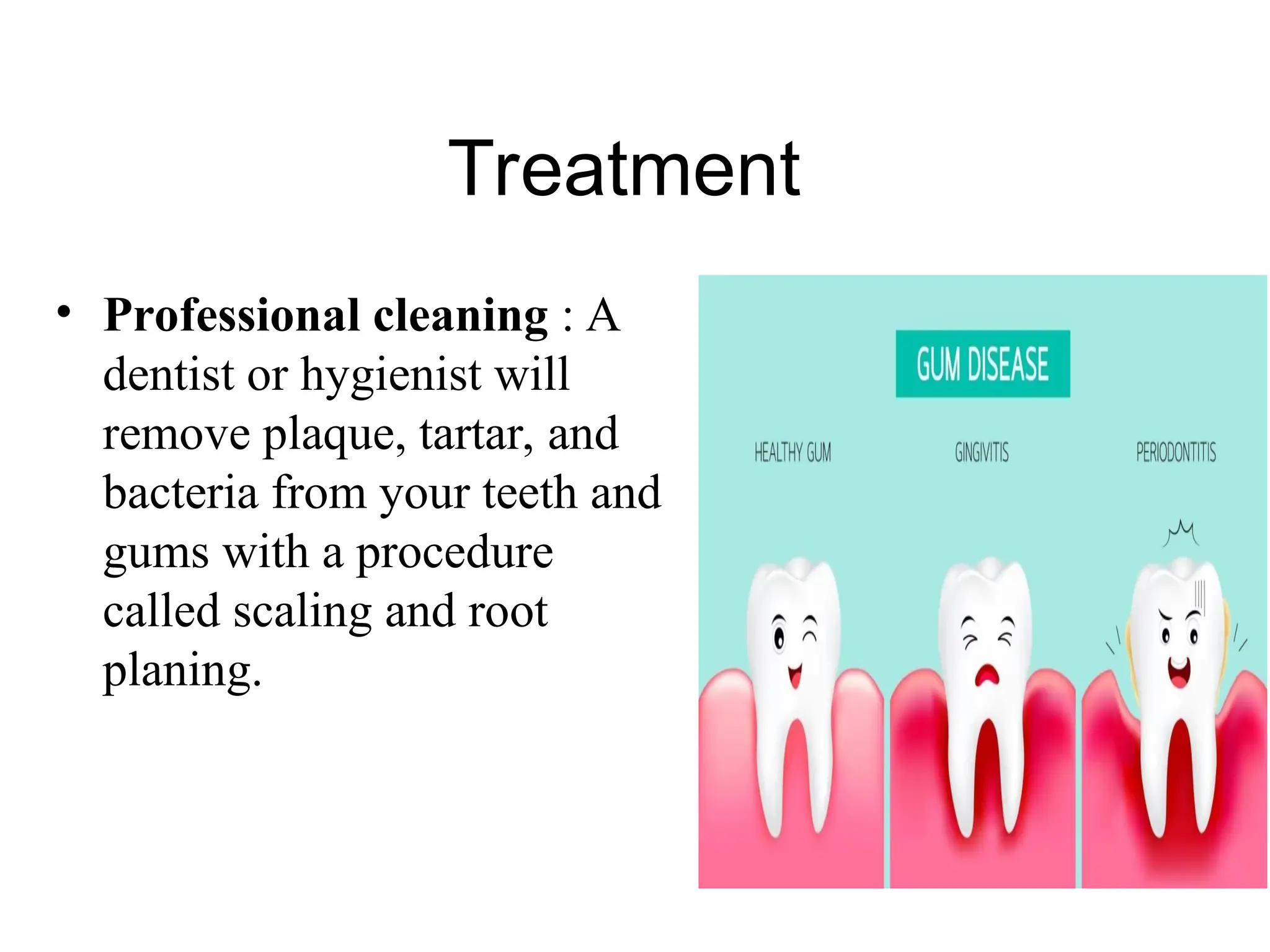
The document provides a comprehensive overview of various mucous membrane disorders, including their types, signs, symptoms, diagnosis, and treatment options. Key conditions discussed include cheilitis, stomatitis, and gingivitis, each associated with distinct causes and management strategies. The information aims to equip nursing students with essential knowledge about these medical conditions.