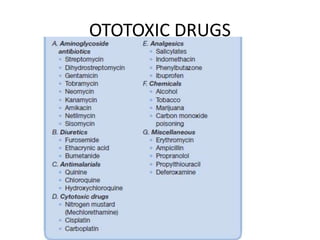
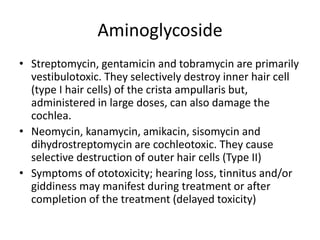
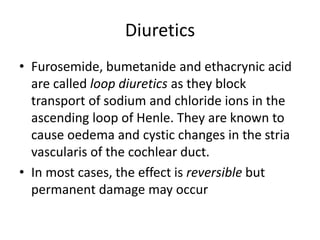
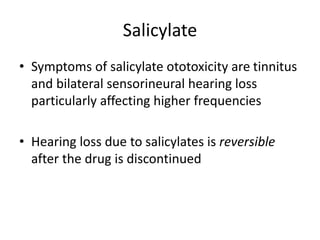
This document discusses ototoxicity, which is damage to the inner ear caused by exposure to toxic agents like certain drugs. It defines cochleotoxicity as damage to the cochlea resulting in hearing loss and tinnitus, while vestibulotoxicity damages the vestibule and can cause vertigo. Common ototoxic drugs mentioned are aminoglycosides like streptomycin which damage hair cells, diuretics which can cause edema in the cochlea, salicylates and quinine which can both reversibly cause tinnitus and hearing loss, and cytotoxic drugs like cisplatin which damage outer hair cells and cause high frequency hearing loss. Management strategies include discontinuing the toxic drug,