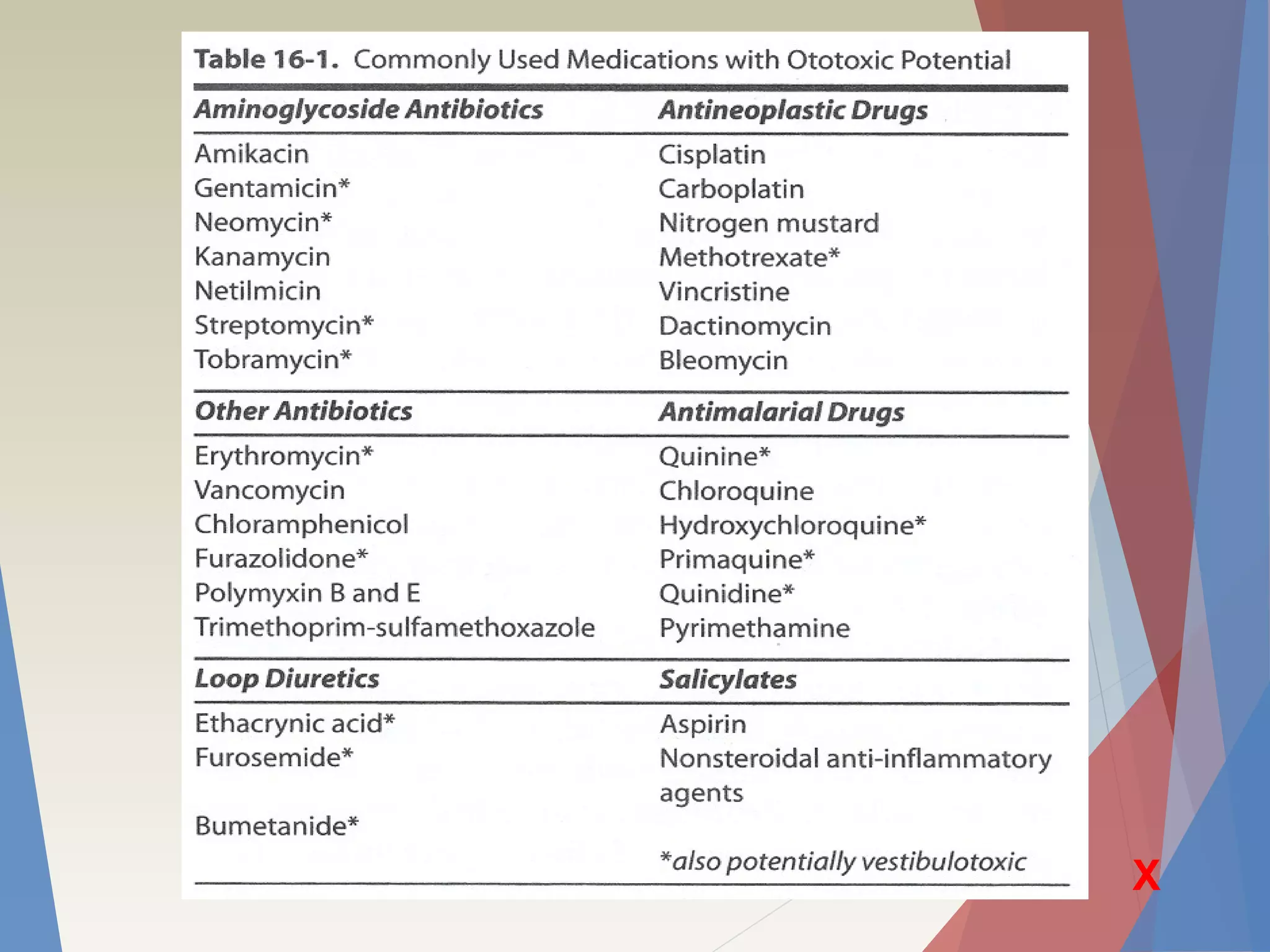
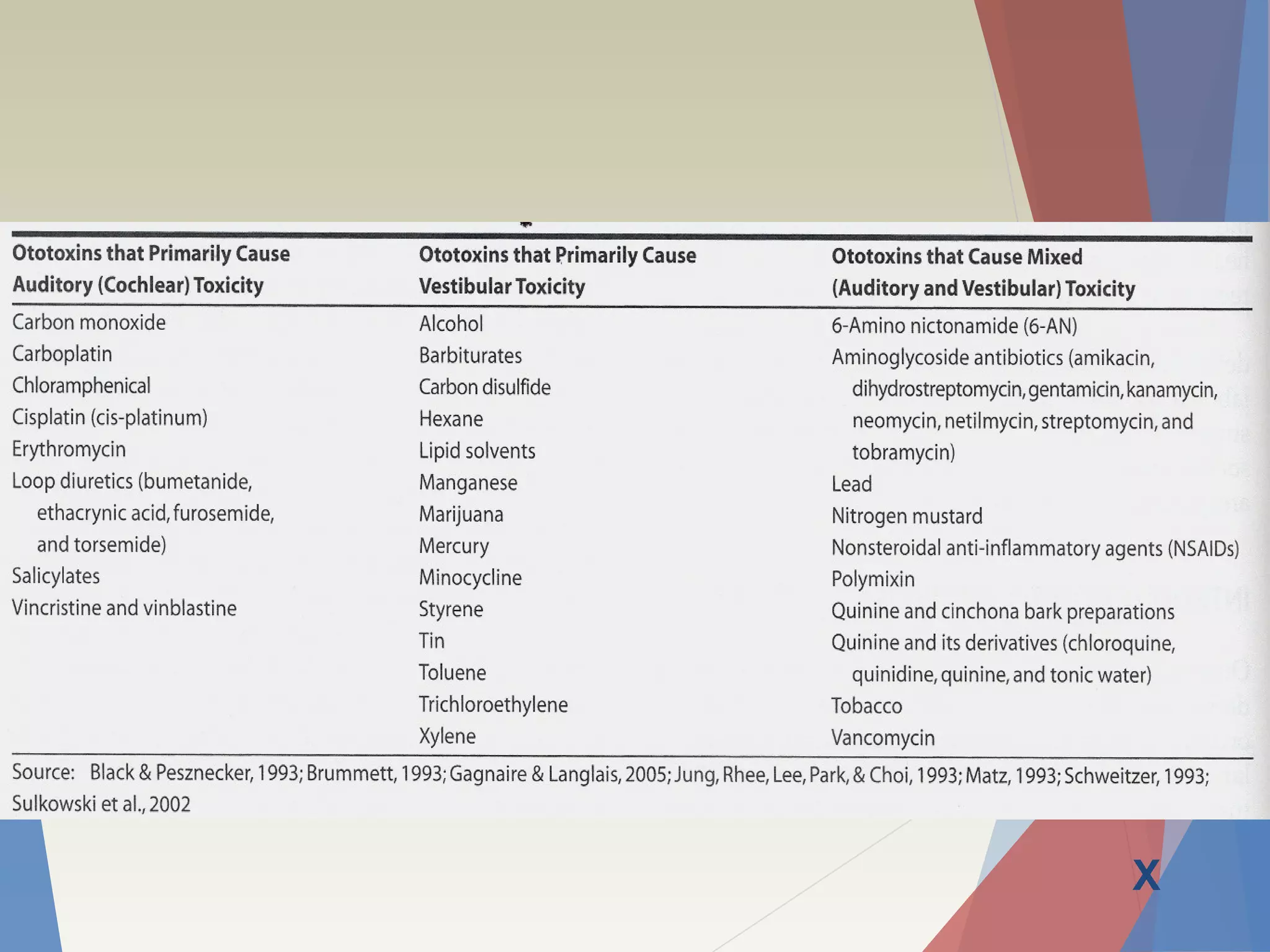
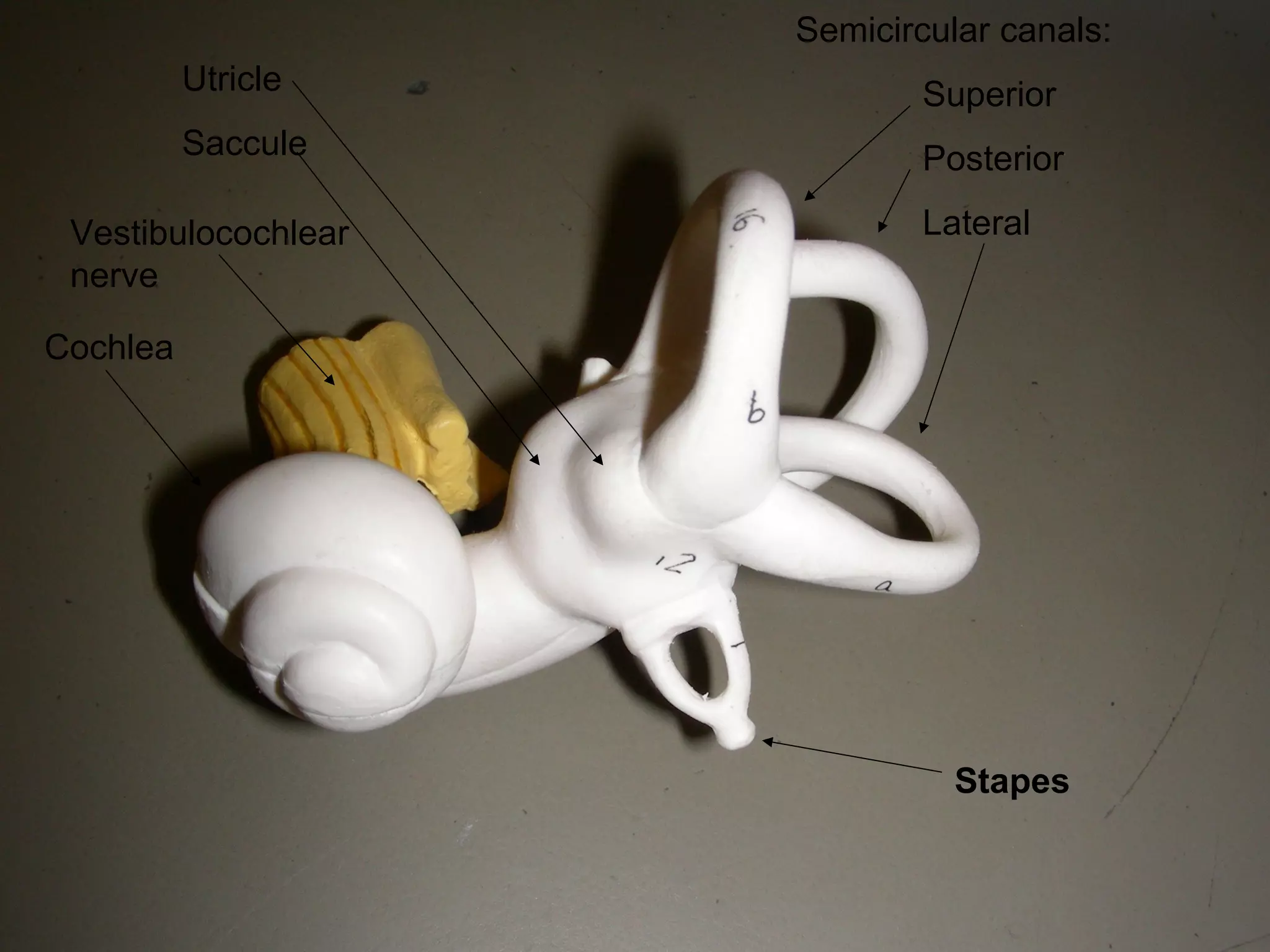
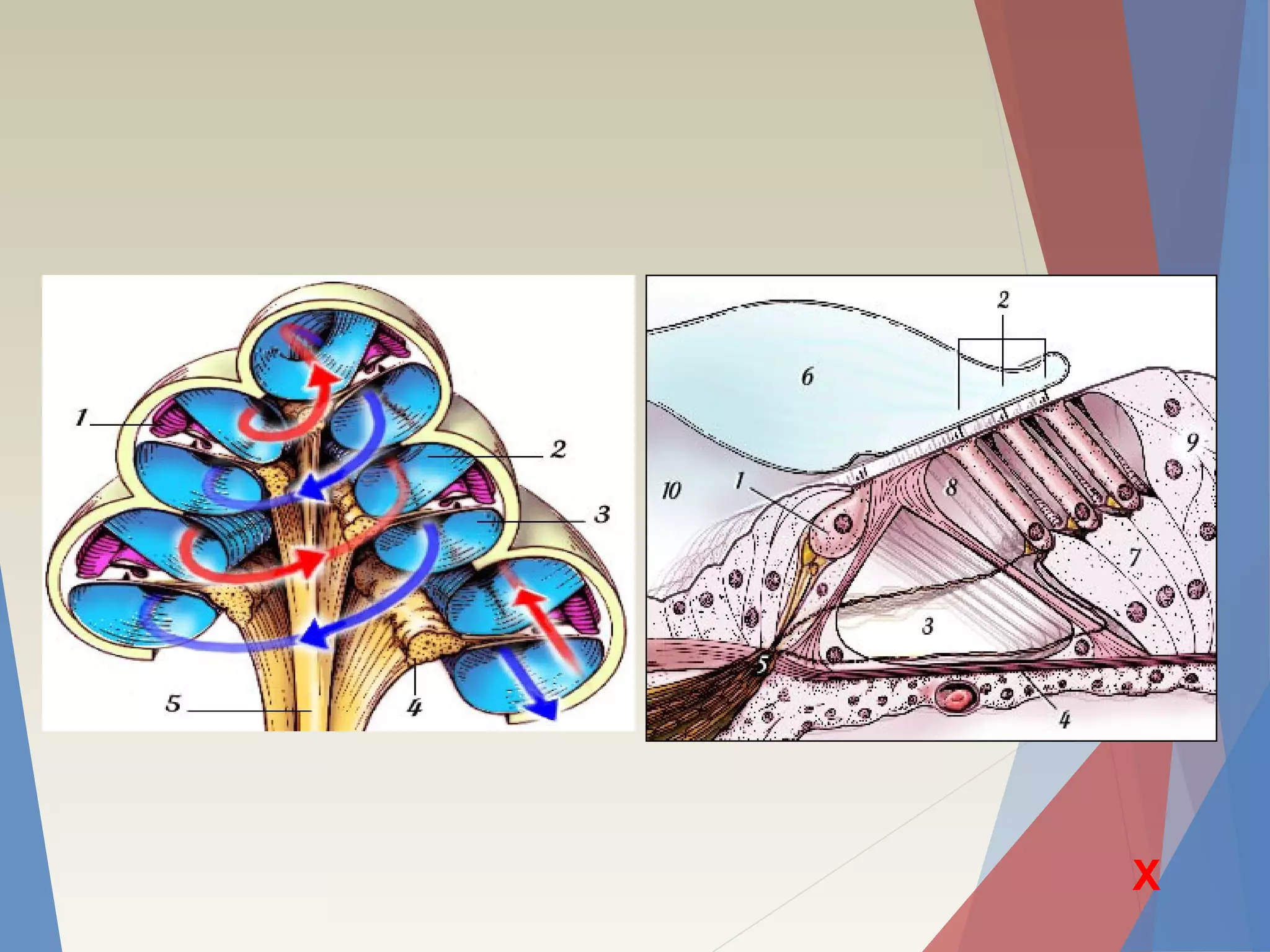
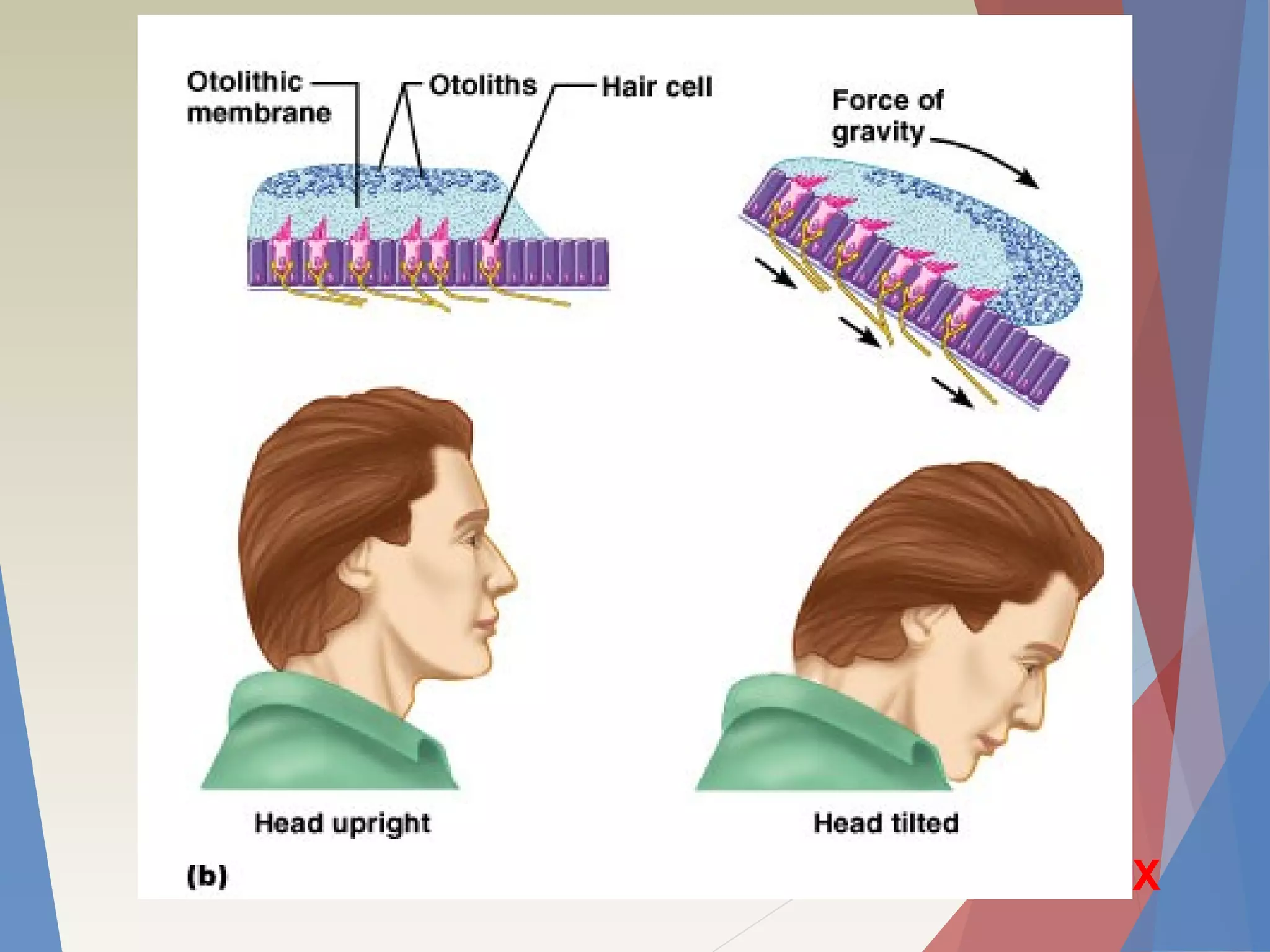
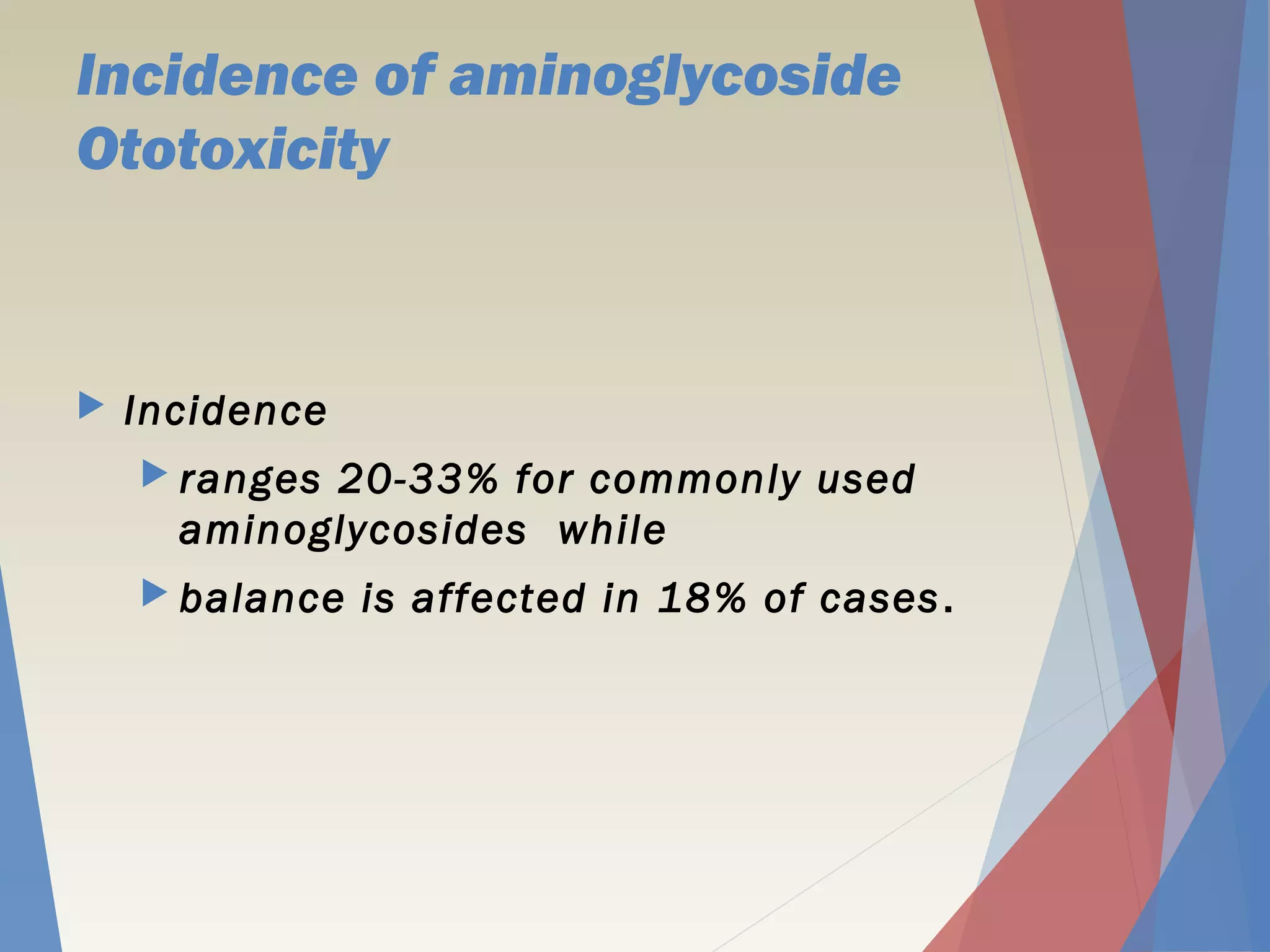
Certain medications like aminoglycoside antibiotics and chemotherapy drugs can damage hearing and balance by harming delicate inner ear cells. Regular audiometric monitoring above 8 kHz, where hearing is lost first, is the most effective way to detect this potentially preventable ototoxicity early. Protective strategies are being studied to allow safer use of these important drugs.