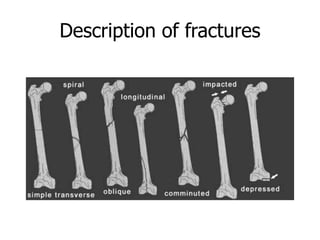
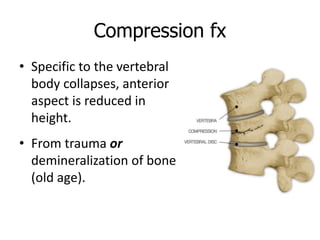
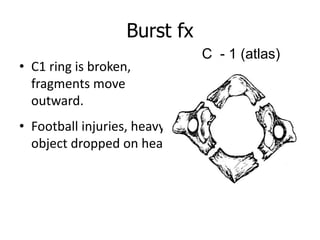
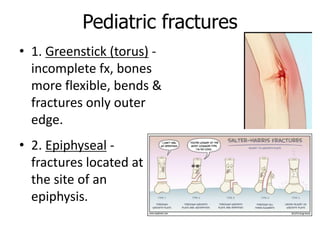
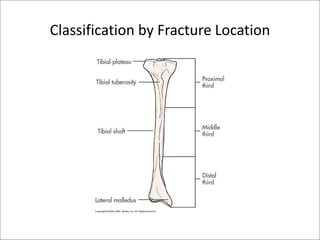
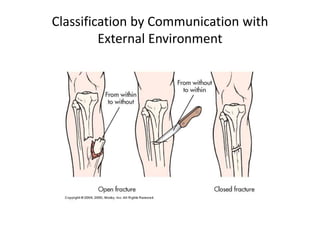
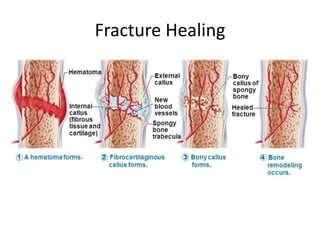
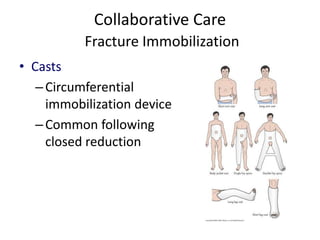
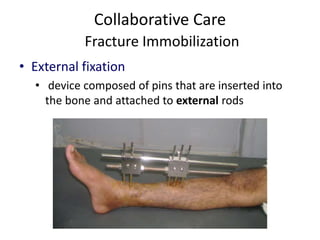
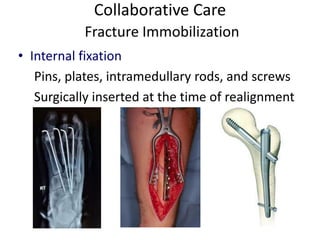
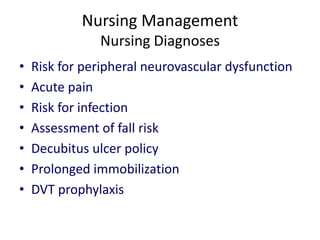
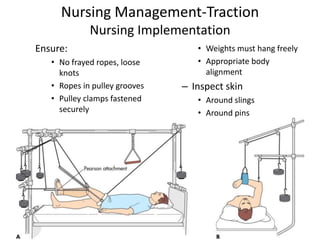
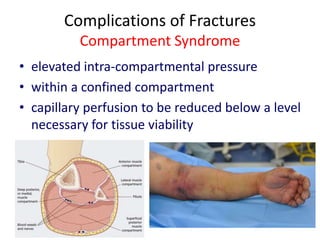
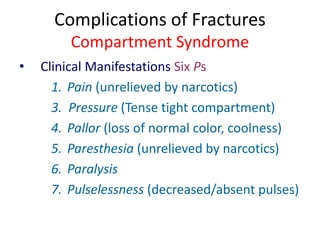
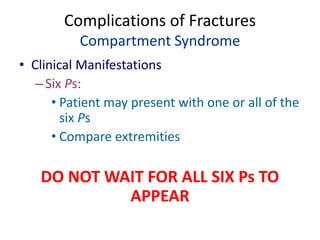
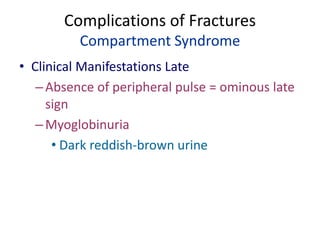
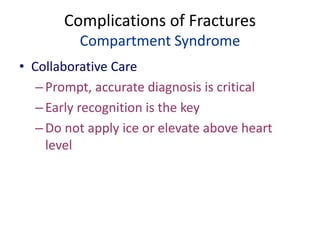
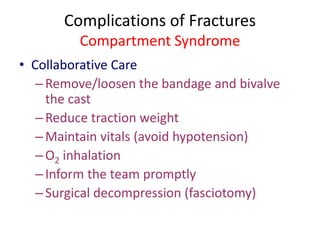
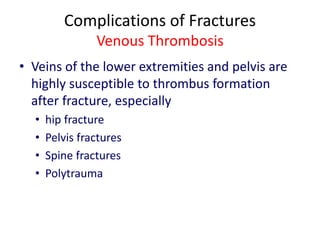
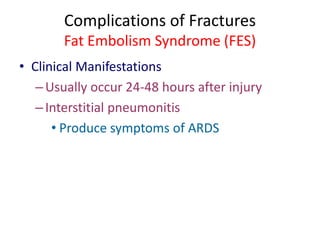
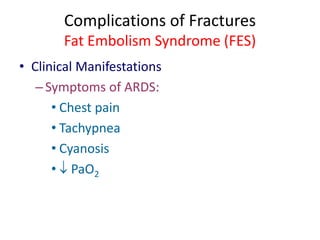
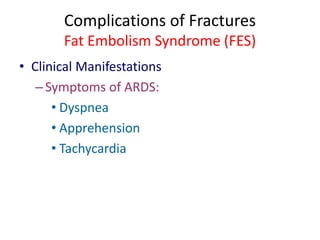
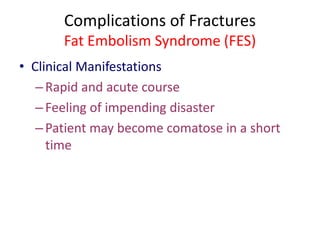
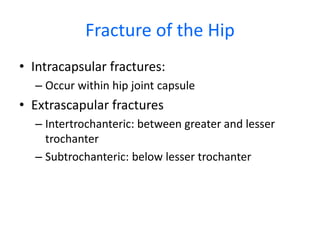
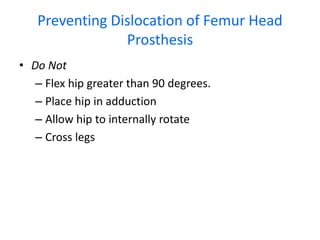
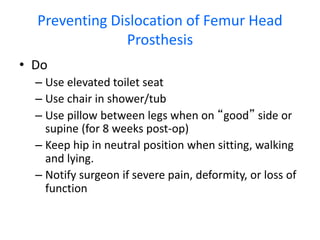
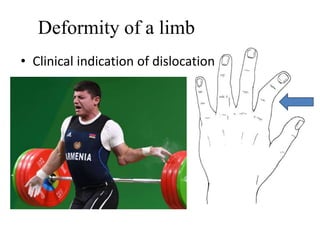
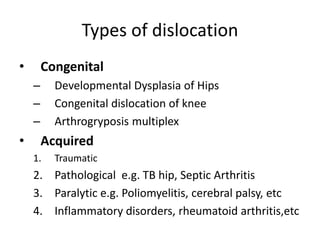
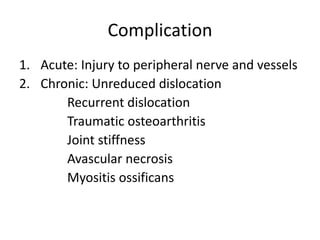
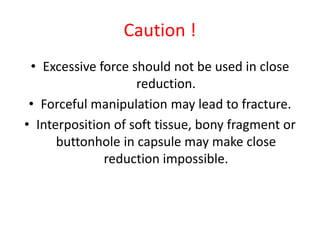
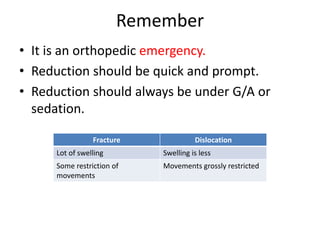
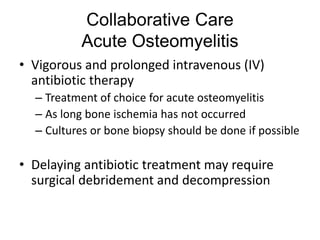
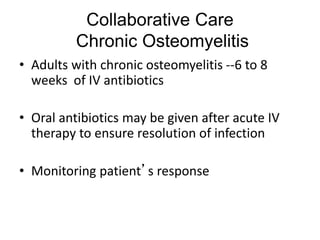
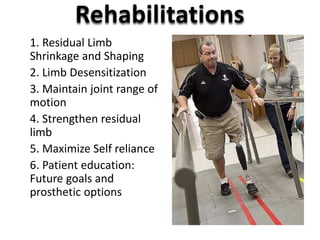
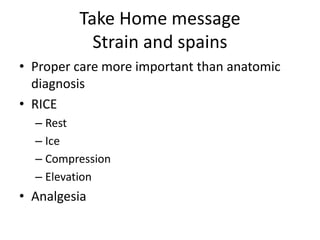
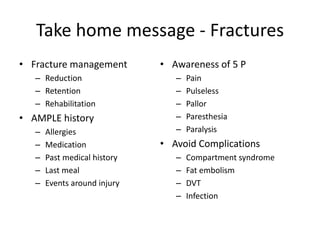
This document provides an overview of the management of musculoskeletal trauma and problems. It discusses various topics including fractures, joint dislocations, contusions, sprains, strains, osteomyelitis, and low back pain. For fractures specifically, it describes the types of fractures, clinical manifestations, diagnostic tests, management including reduction, immobilization, and nursing care. It also discusses complications that can arise from fractures like infection, compartment syndrome, venous thrombosis, and fat embolism syndrome. Treatment for hip fractures is also outlined.