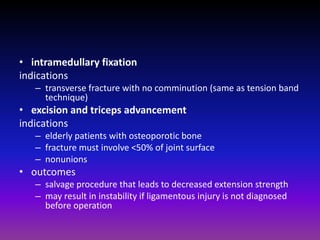
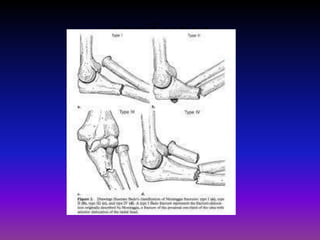
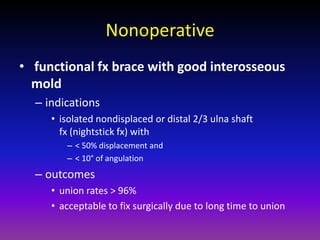
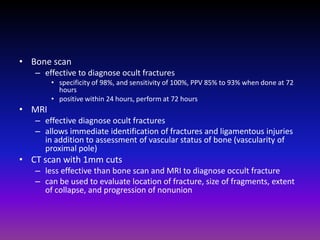
The document discusses various fractures of the upper limb, including: pulled elbow in children, fractures of the proximal radius (head, neck), Monteggia and Galeazzi fractures involving the forearm bones and dislocations, fractures of both bones of the forearm, distal radius fractures including Colles' fracture, and scaphoid fractures. Treatment options depend on the type and location of the fracture, and may involve closed reduction, casting, external fixation, plating, or intramedullary nailing. Complications include nonunion, malunion, neurovascular injuries, and arthritis.