This document provides an overview of musculoskeletal trauma, including:
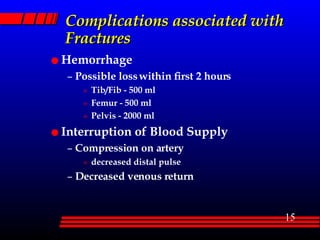
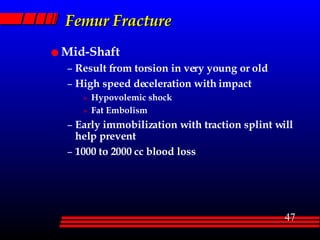
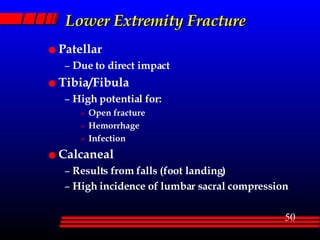
1) Musculoskeletal injuries occur in 70-80% of multi-trauma patients and can range from minor impairments to life-threatening injuries like pelvic or femur fractures.
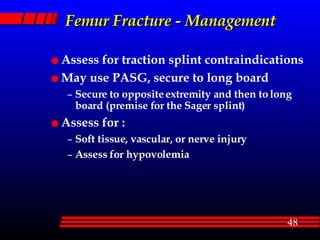
2) A thorough musculoskeletal assessment involves evaluating the six P's (pain, pallor, paresthesia, pulses, paralysis, pressure) as well as inspection and palpation of injuries.
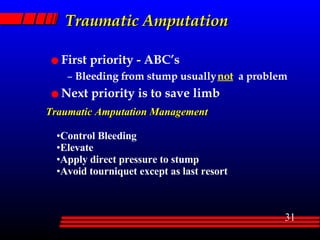
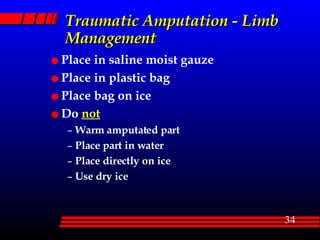
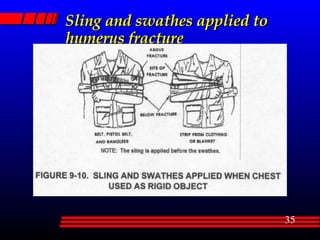
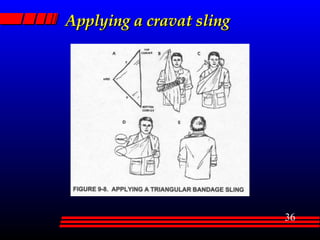
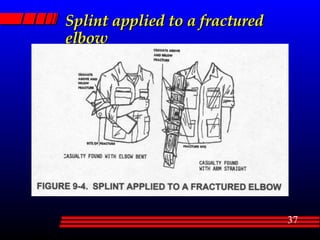
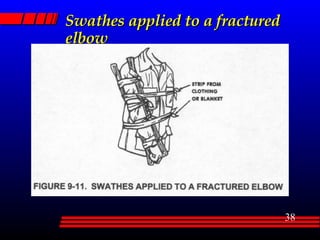
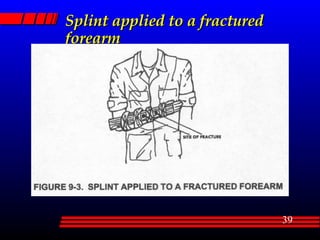
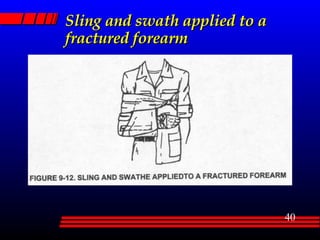
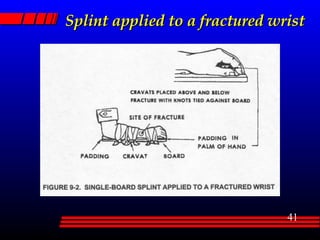
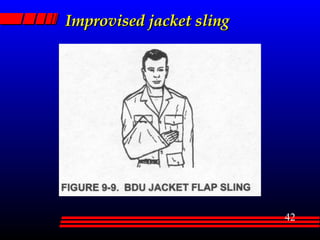
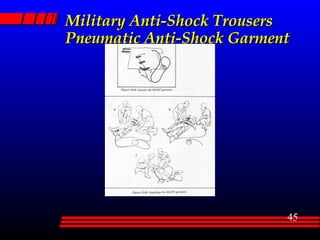
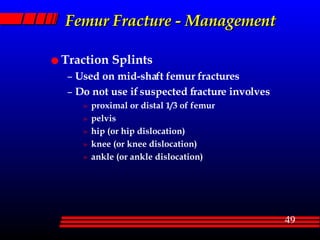
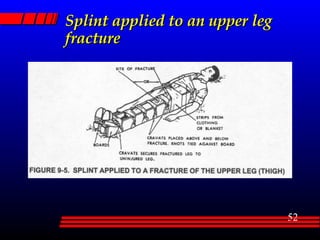
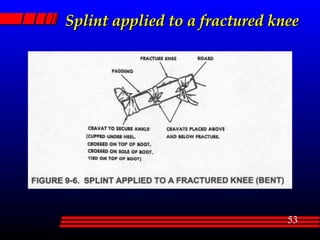
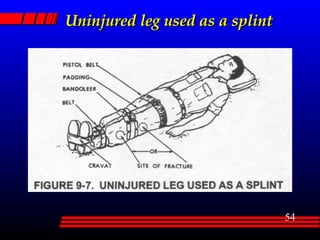
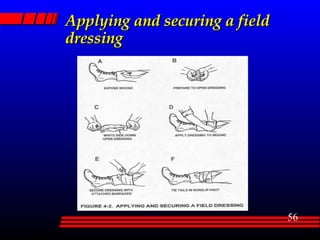
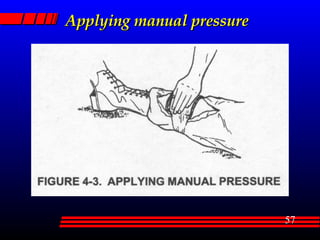
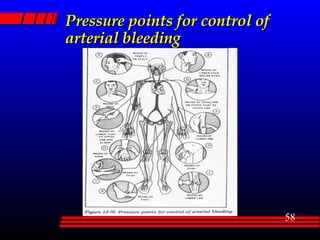
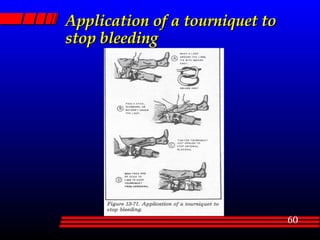
3) Initial management of musculoskeletal trauma focuses on immobilization, hemorrhage control, and splinting fractures to prevent further injury while stabilizing the patient for transport.