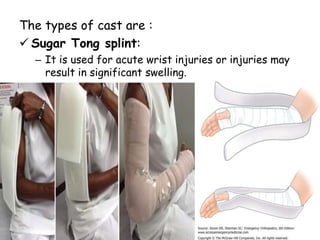
The document discusses fractures, including their definition, incidence, risk factors, pathophysiology, healing process, clinical manifestations, classification, diagnostic evaluation, and management. Fractures are breaks in bone continuity that can be caused by trauma or weakened bone. Evaluation involves history, exam, and imaging like x-rays. Treatment focuses on reduction, immobilization, and rehabilitation to heal the fracture and restore function.