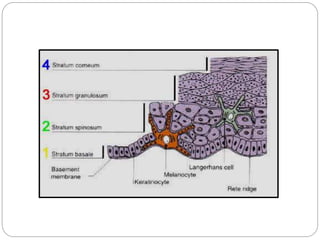
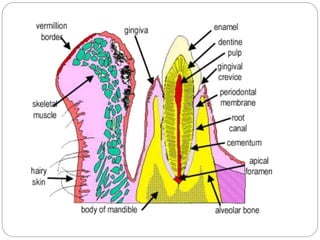
This document provides information on the oral mucous membrane (OMM). It defines OMM as the moist lining of the oral cavity that communicates with the exterior. The OMM consists of two layers - an epithelial layer and an underlying connective tissue layer. It is classified based on function into masticatory mucosa, lining mucosa, and specialized mucosa. Histologically, the OMM contains keratinized and non-keratinized epithelium made up primarily of keratinocytes and some non-keratinocytes like melanocytes and Langerhans cells. The document describes the microscopic structure of the different layers in keratinized and non-keratinized epithelium.