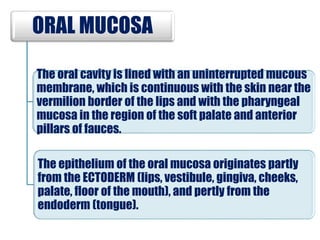
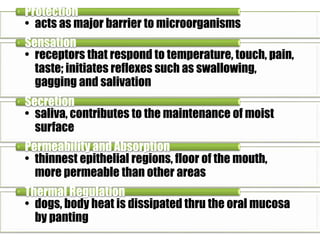
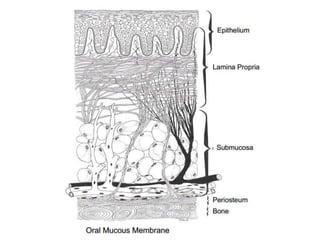
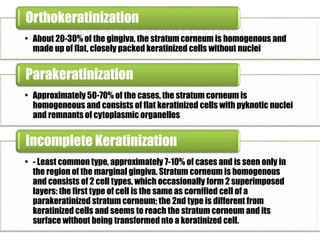
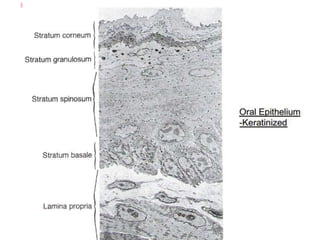
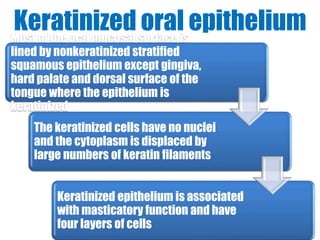
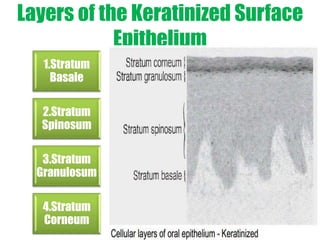
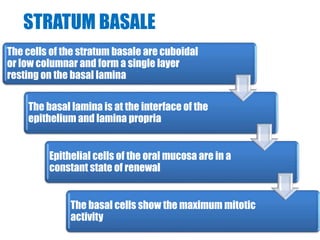
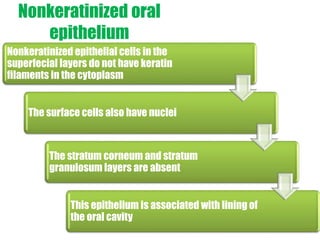
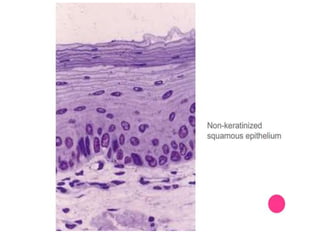
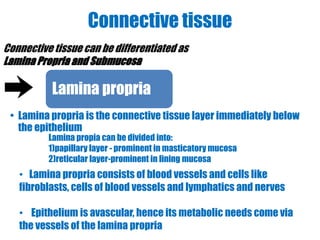
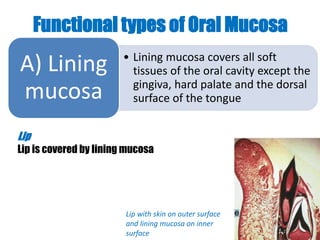
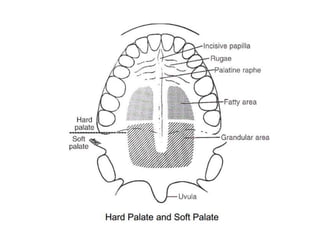
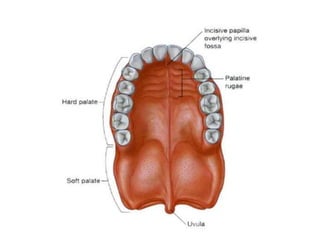
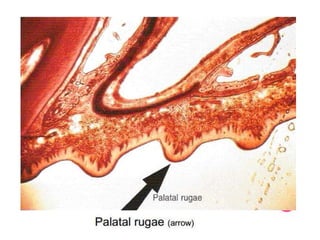
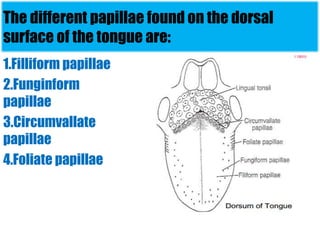
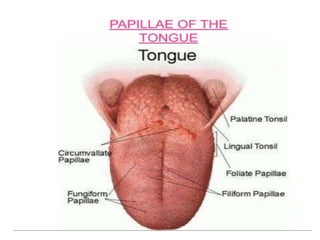
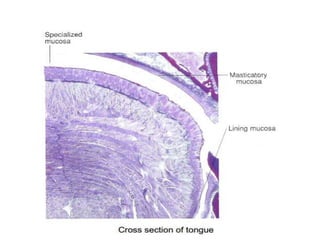
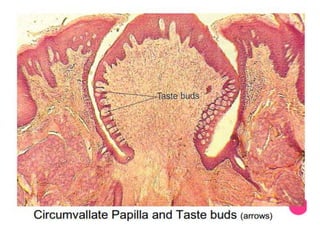
The oral cavity is lined by oral mucosa, which is continuous with the skin and pharyngeal mucosa. The oral mucosa consists of three types - masticatory, lining, and specialized mucosa. Masticatory mucosa covers areas involved in chewing and is keratinized, while lining mucosa covers other soft tissue areas and is non-keratinized. Specialized mucosa covers the dorsal tongue and contains papillae involved in taste. The oral mucosa provides protection, sensation, secretion, permeability and thermal regulation functions.