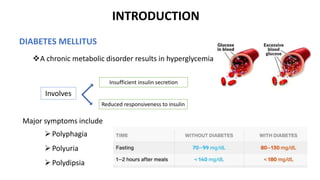
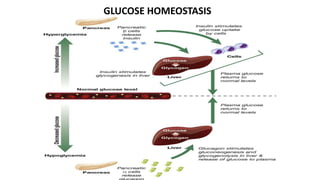
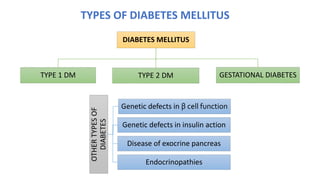
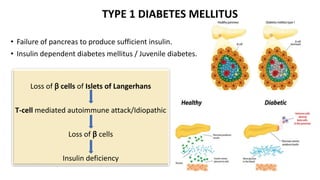
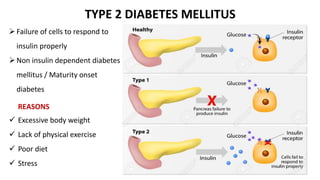
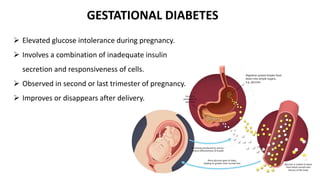
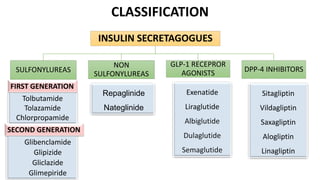
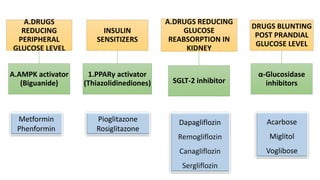
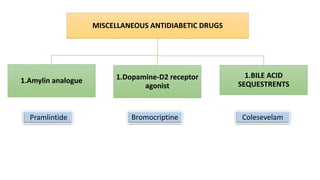
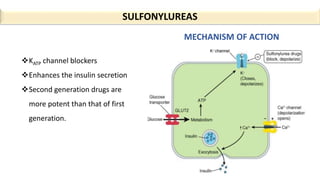
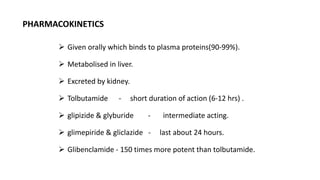
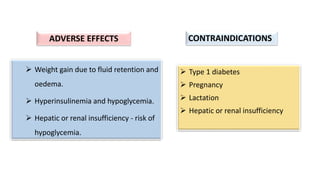
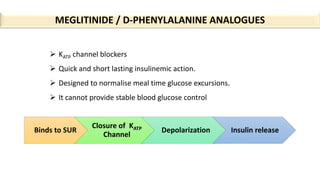
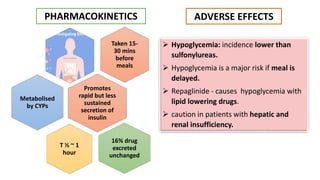
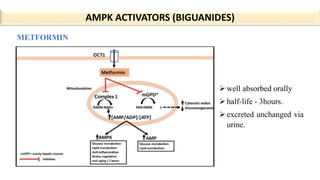
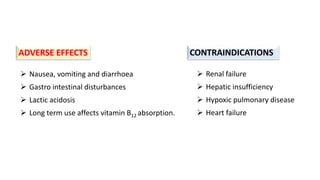
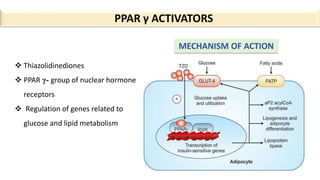
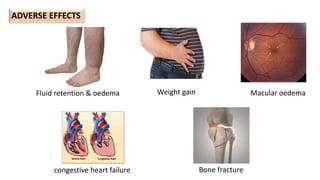
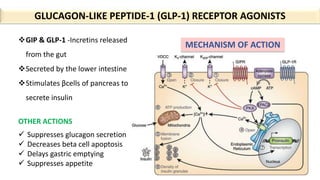
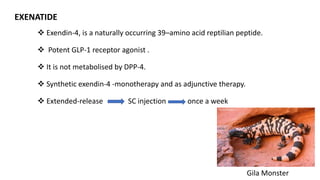
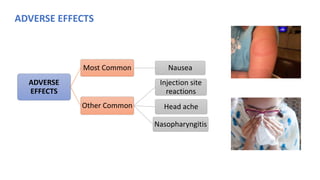
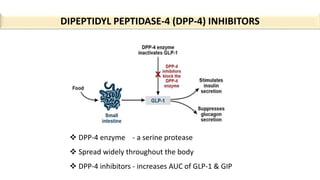
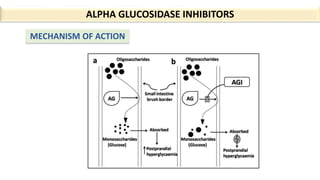
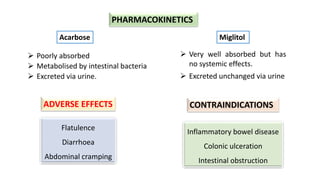
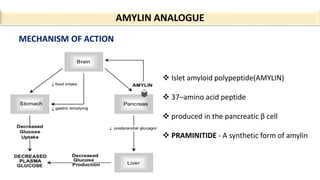
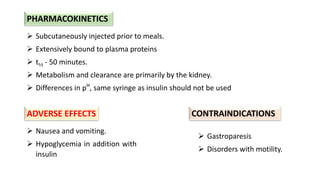
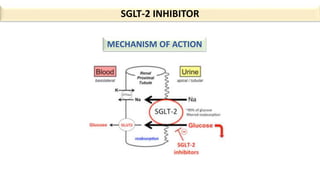
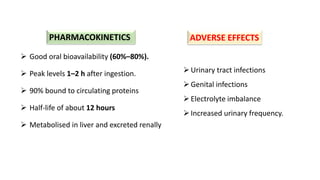
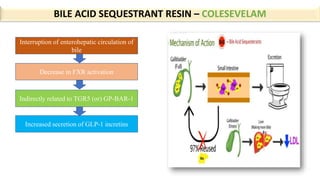
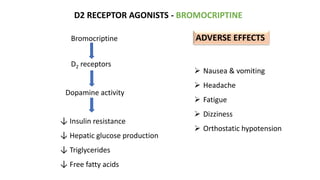
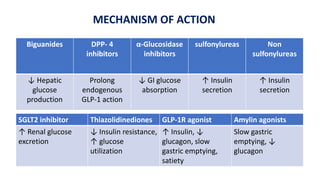
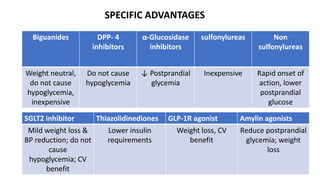
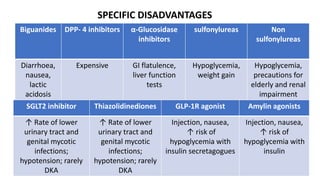
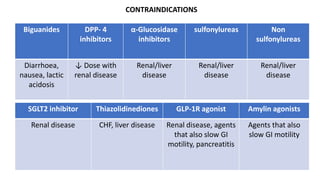
This document provides an overview of oral hypoglycemic agents used to treat diabetes mellitus. It discusses the different types of diabetes and mechanisms of several classes of oral hypoglycemic drugs. The classes covered include sulfonylureas, meglitinides, biguanides, thiazolidinediones, DPP-4 inhibitors, GLP-1 receptor agonists, alpha-glucosidase inhibitors, SGLT2 inhibitors, bile acid sequestrants, and amylin analogues. For each class, the document discusses mechanisms of action, pharmacokinetics, advantages, disadvantages, and contraindications. It concludes that lifestyle modifications and metformin are usually first-line treatments for diabetes