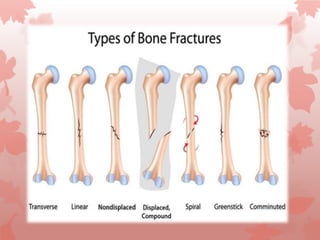
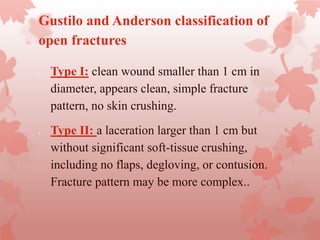
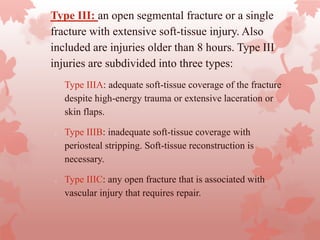
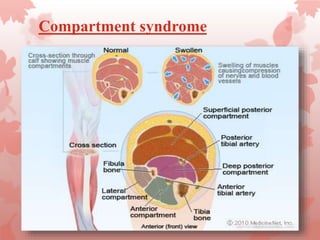
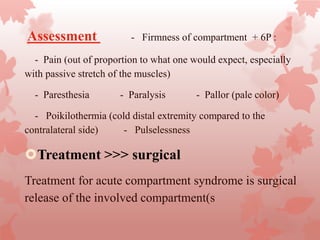
An open fracture is a serious bone fracture where broken bone fragments pierce the skin. Open fractures are caused by high-energy trauma and can lead to infection. They are classified based on wound size and soft tissue damage. Diagnosis involves clinical exam, imaging, and assessing neurovascular status. Management includes wound cleaning, temporary stabilization, antibiotics, and definitive fixation once the wound is healthy. Complications can include infection, neurovascular injury, and compartment syndrome.