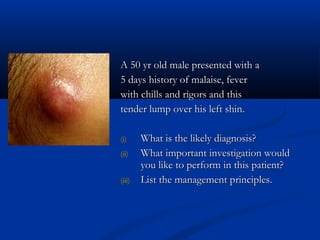
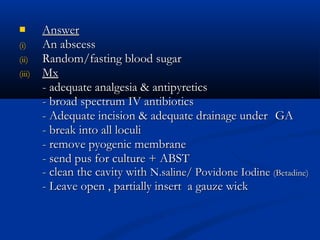
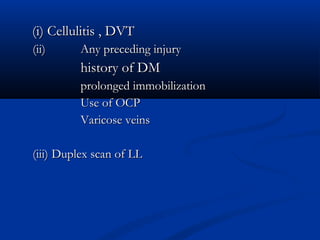
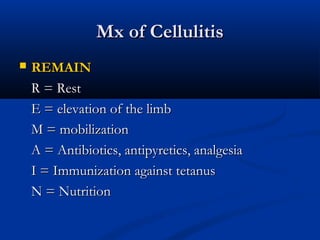
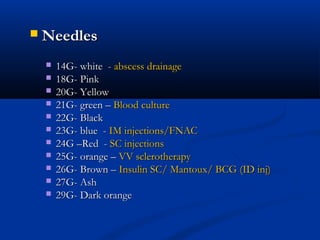
The document describes a 50-year-old male who presented with a tender lump on his left shin and symptoms of fever and malaise for 5 days. The likely diagnosis is an abscess. Important investigations would include a blood sugar test. Management principles are adequate analgesia, antibiotics, adequate incision and drainage of the abscess under general anesthesia, cleaning and dressing of the wound.