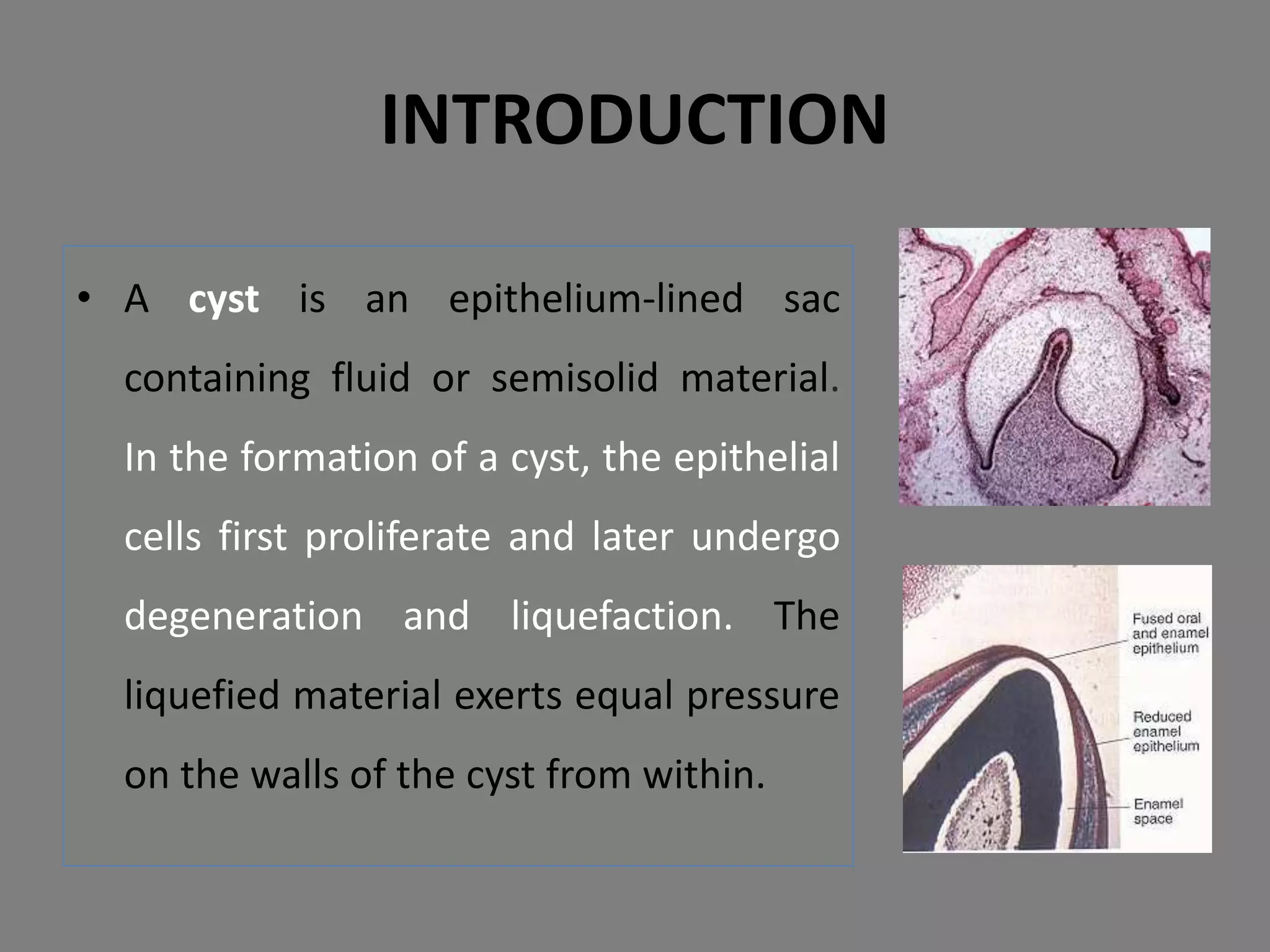
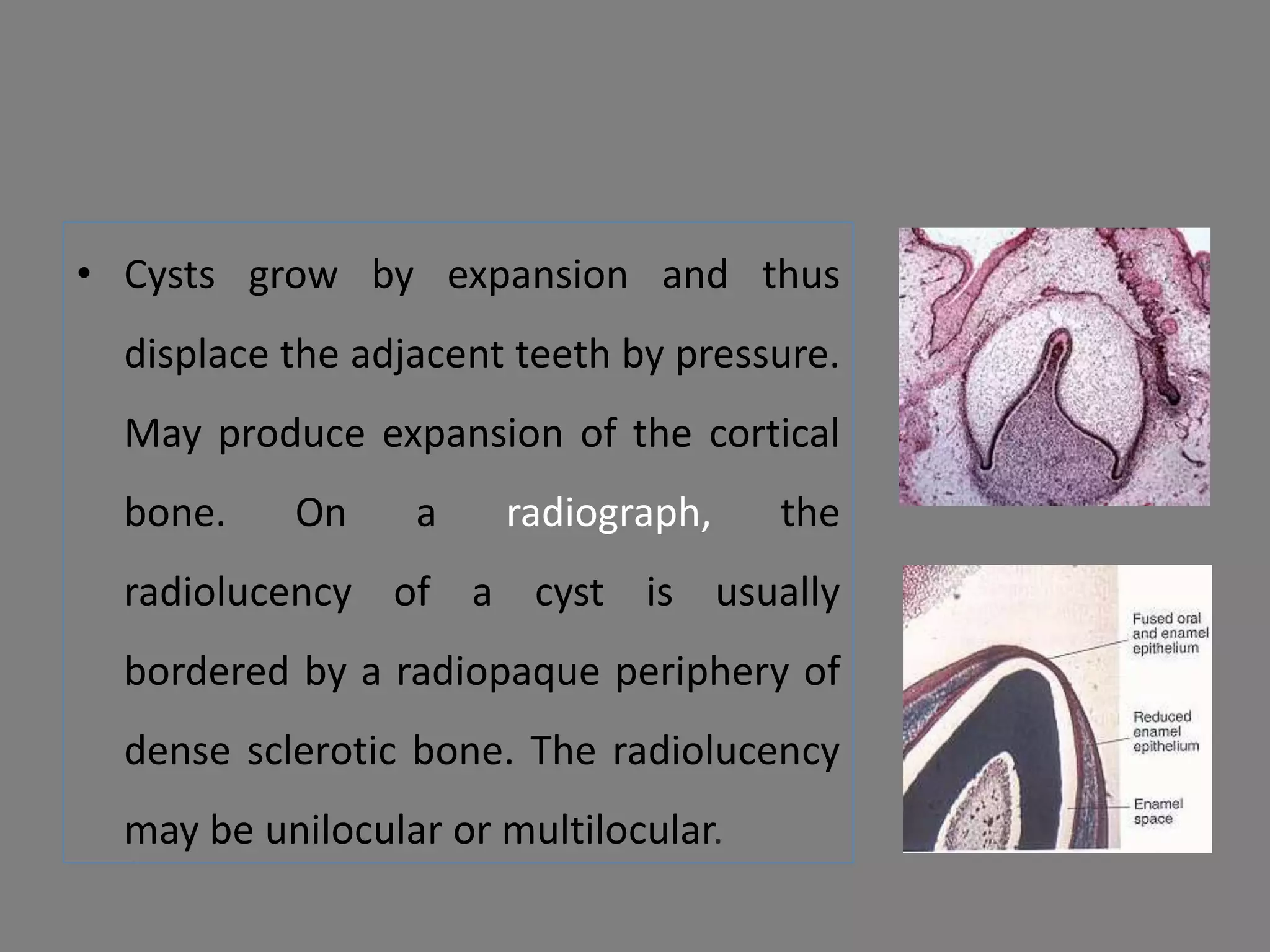
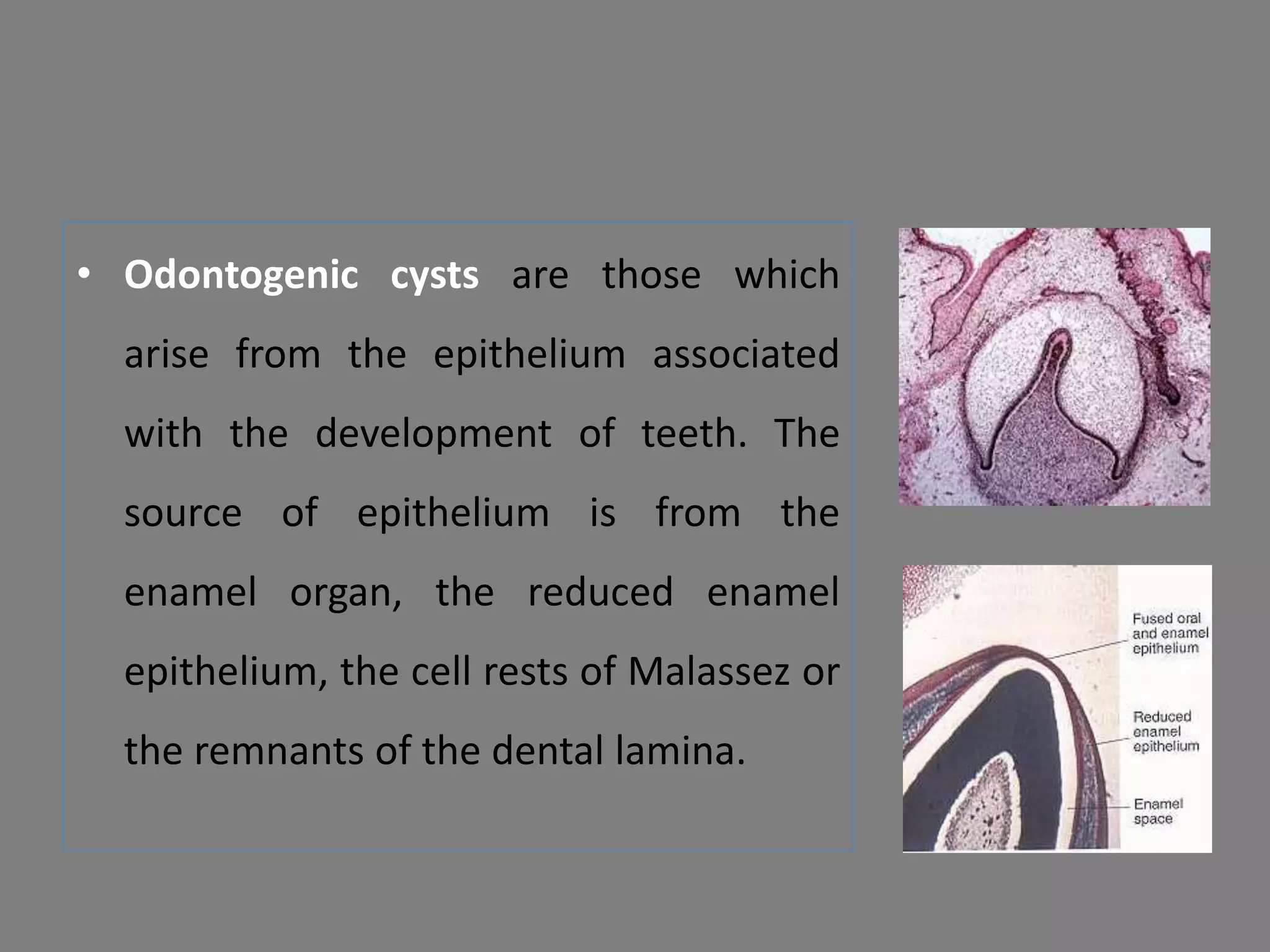
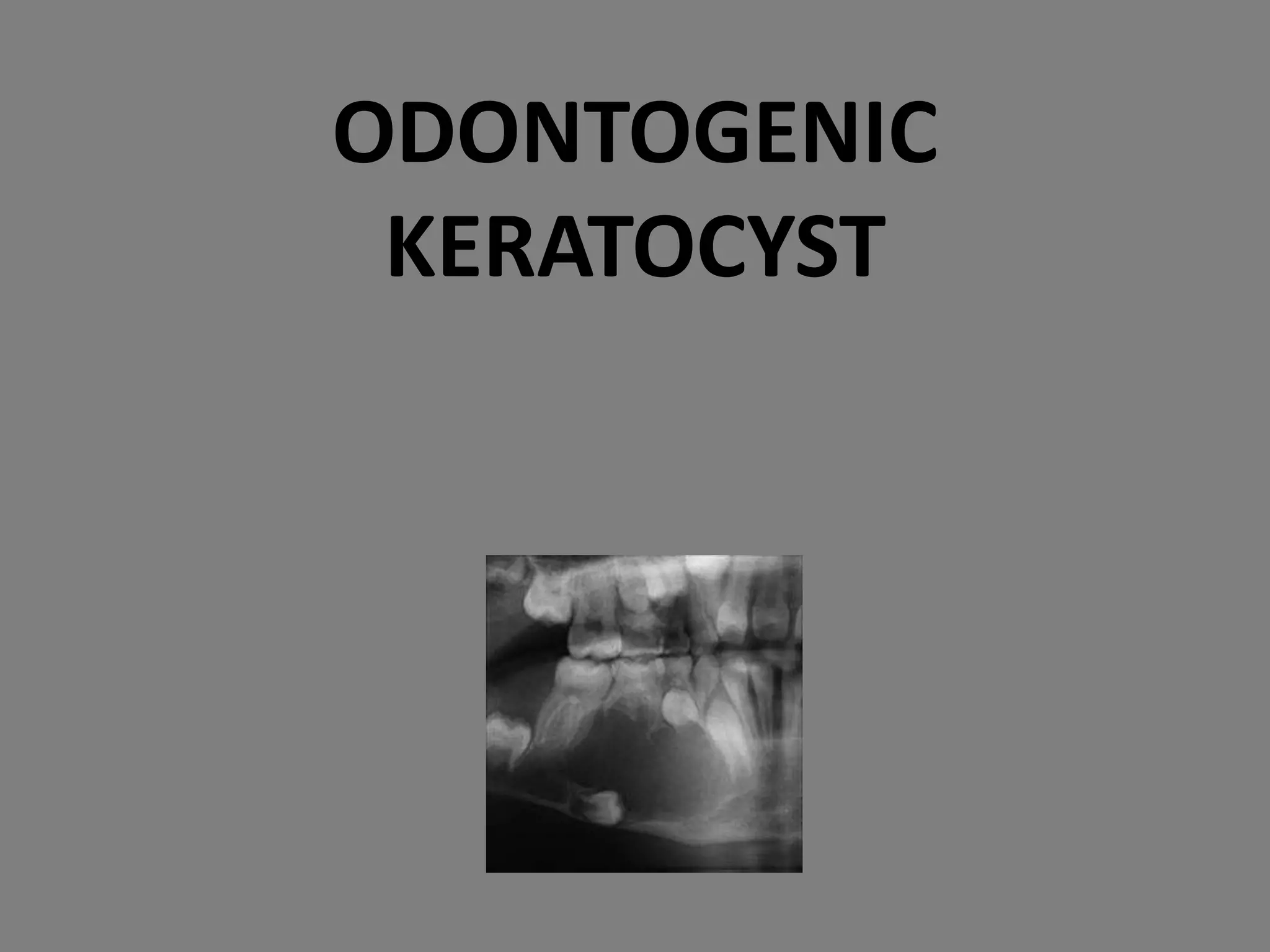
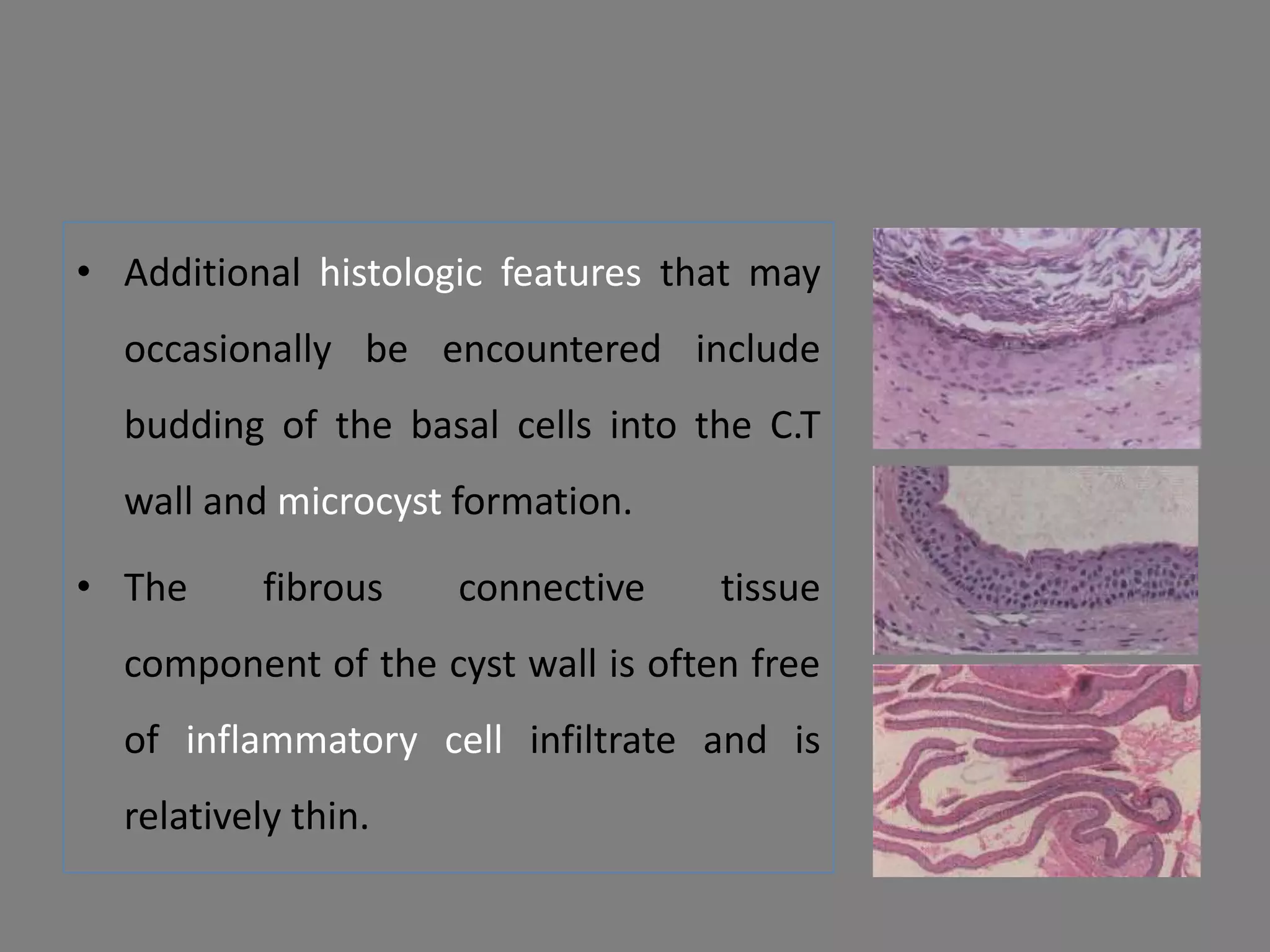
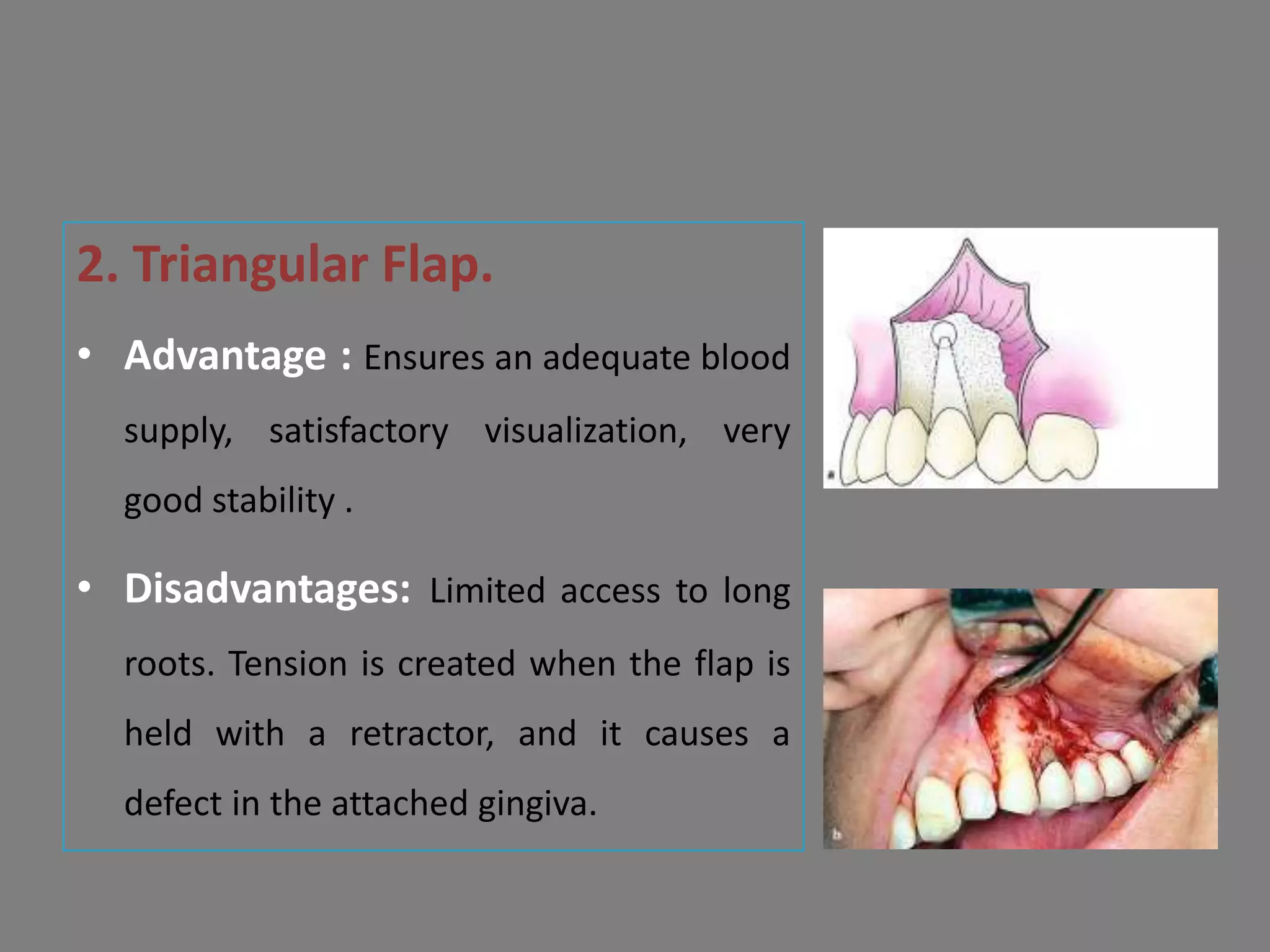
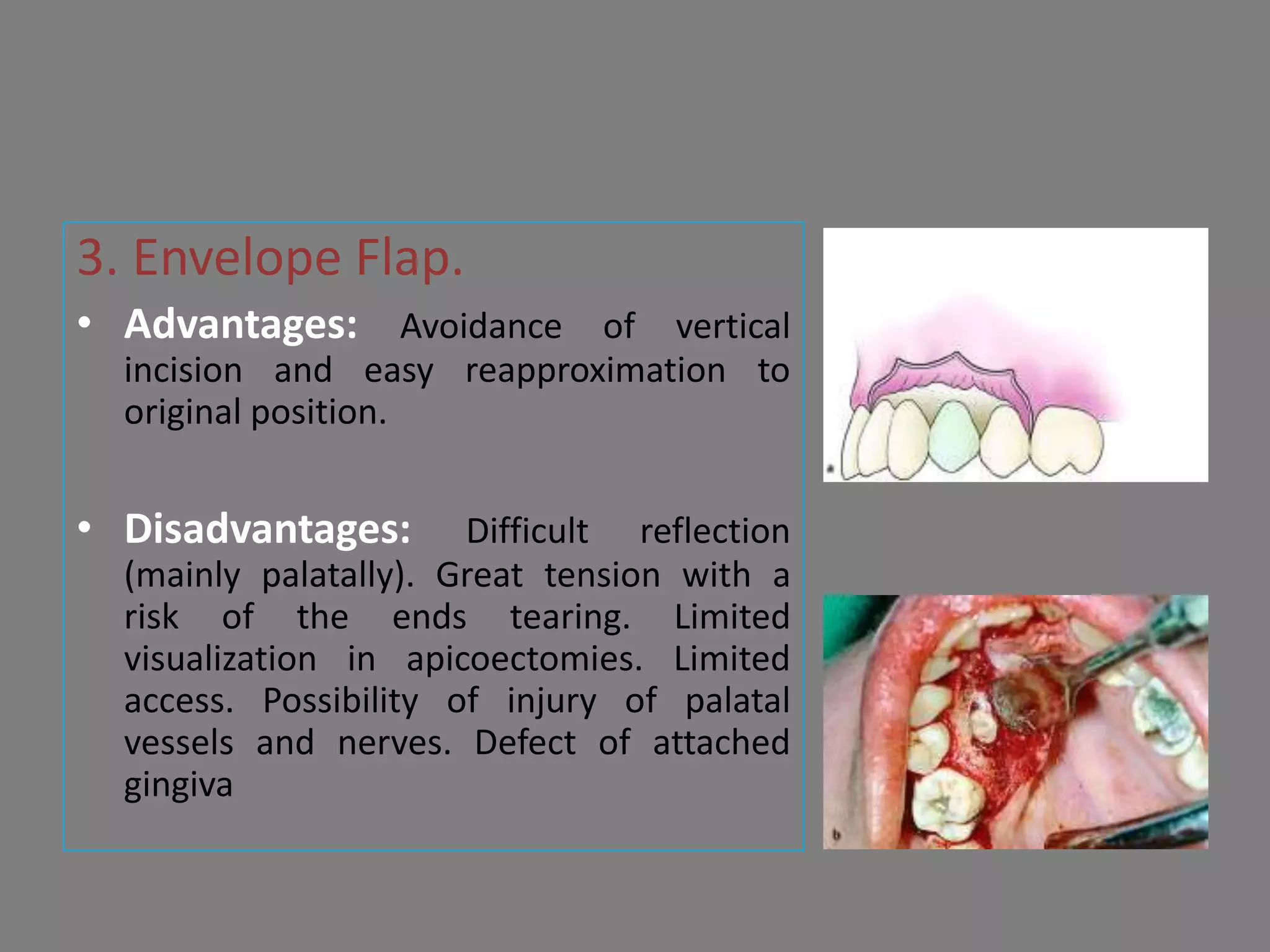
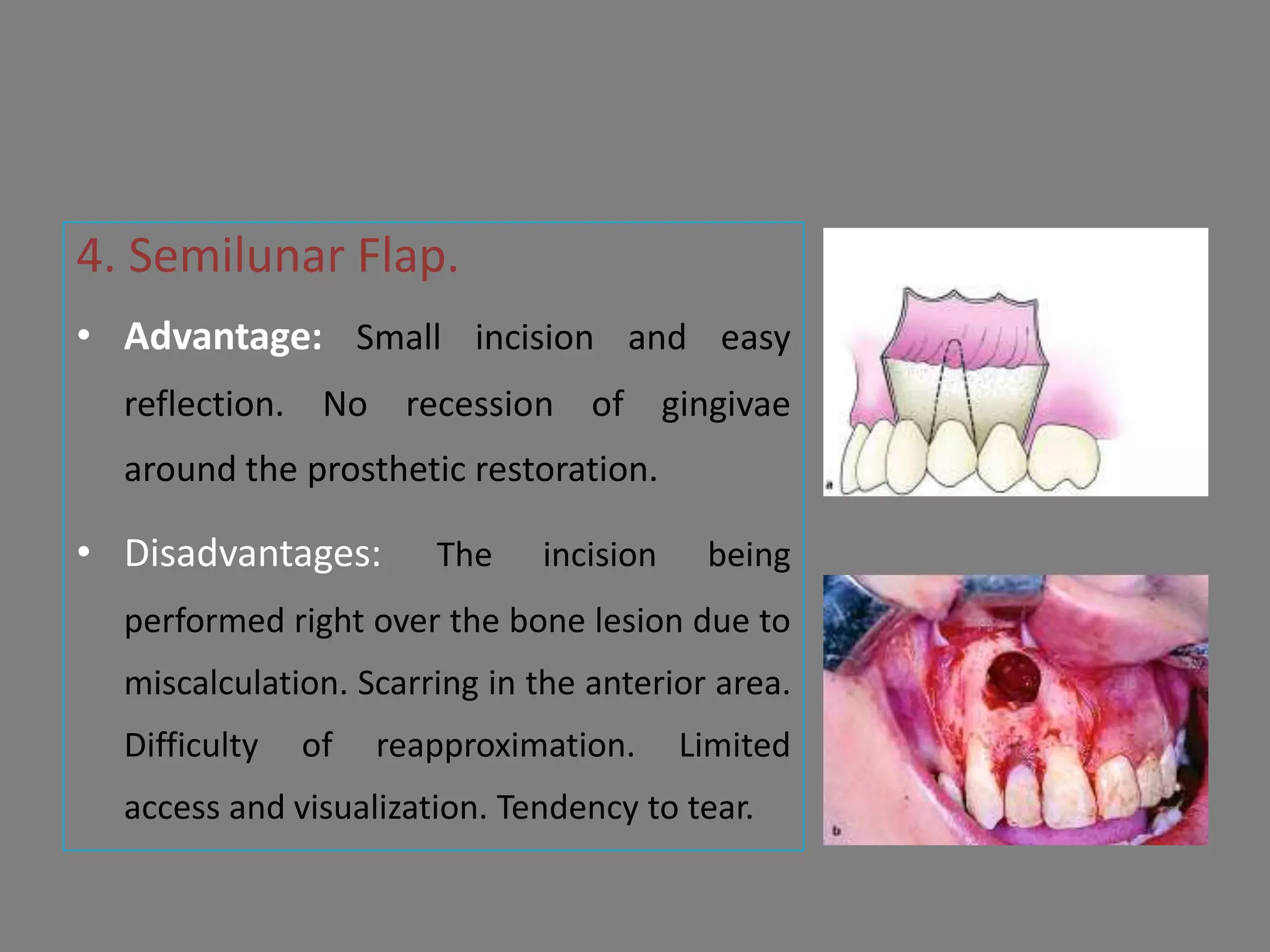
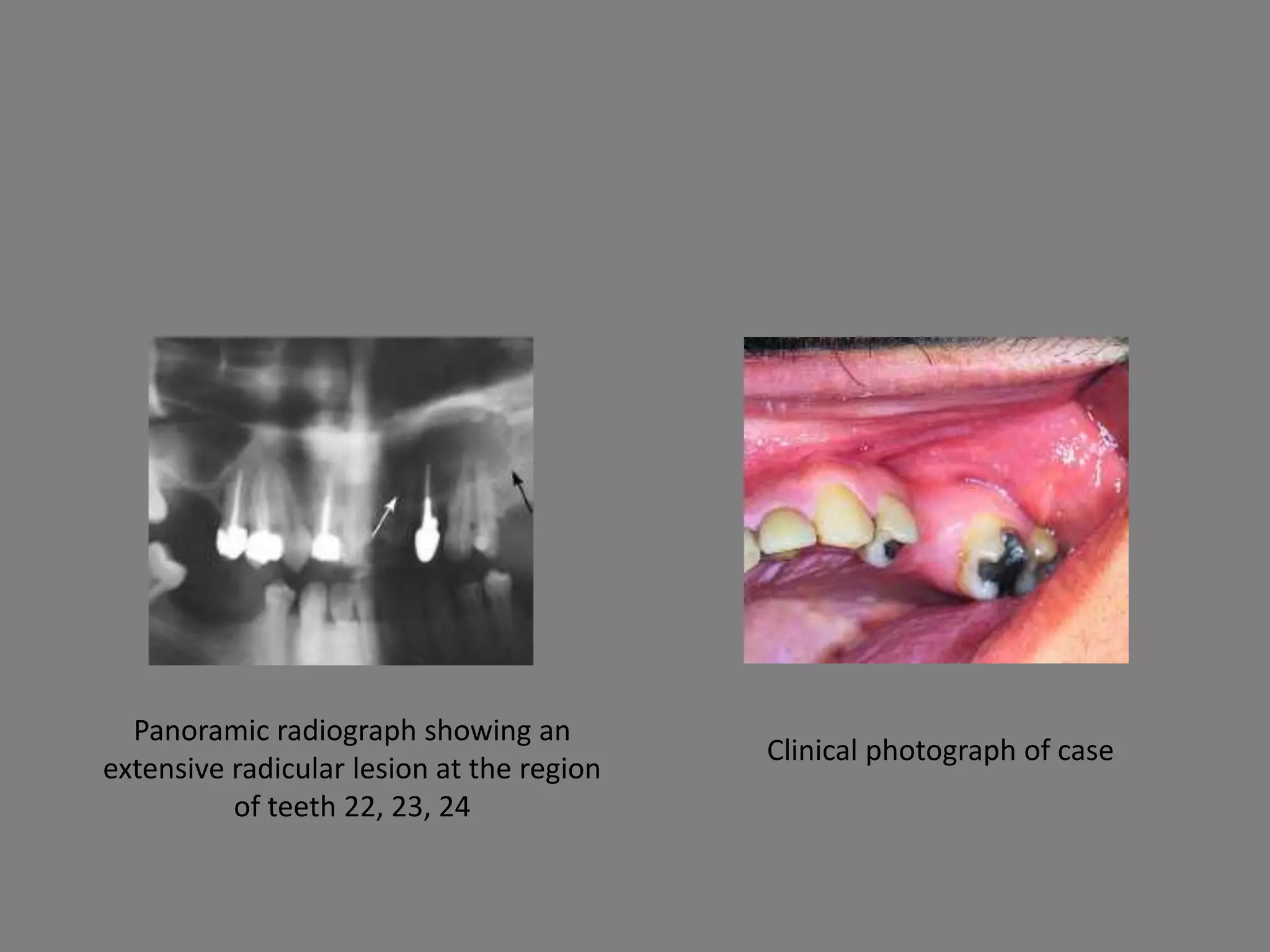
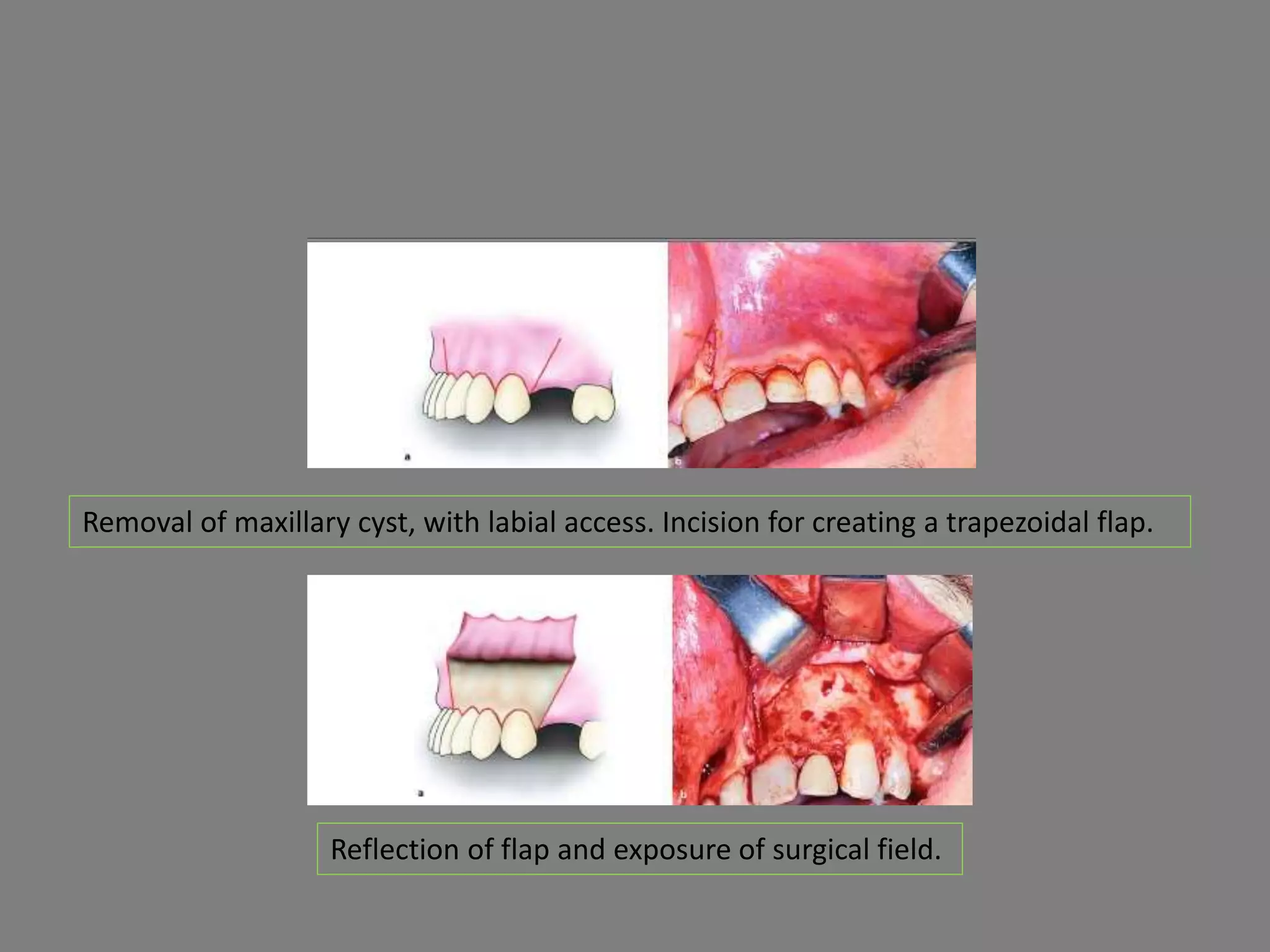
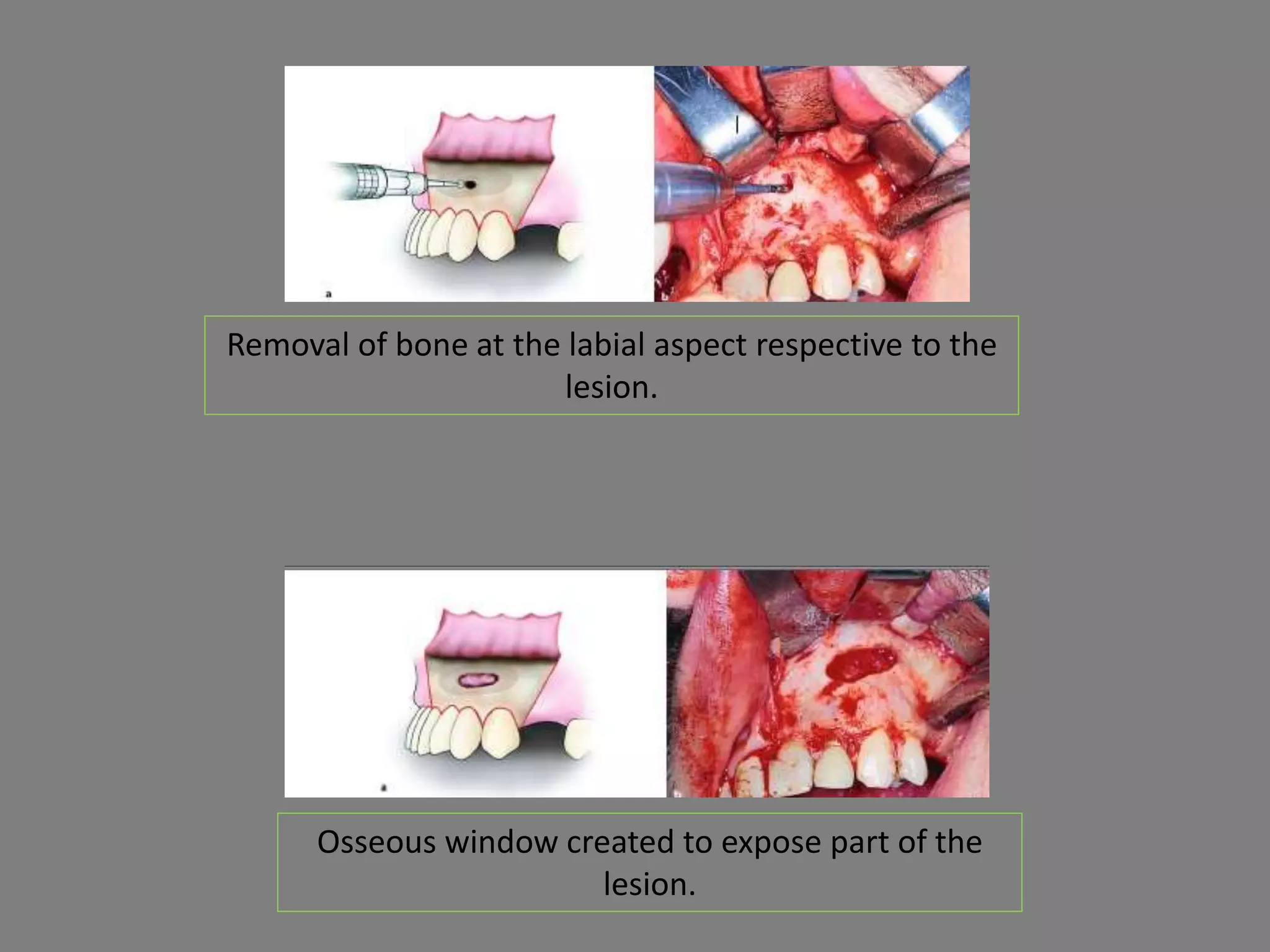
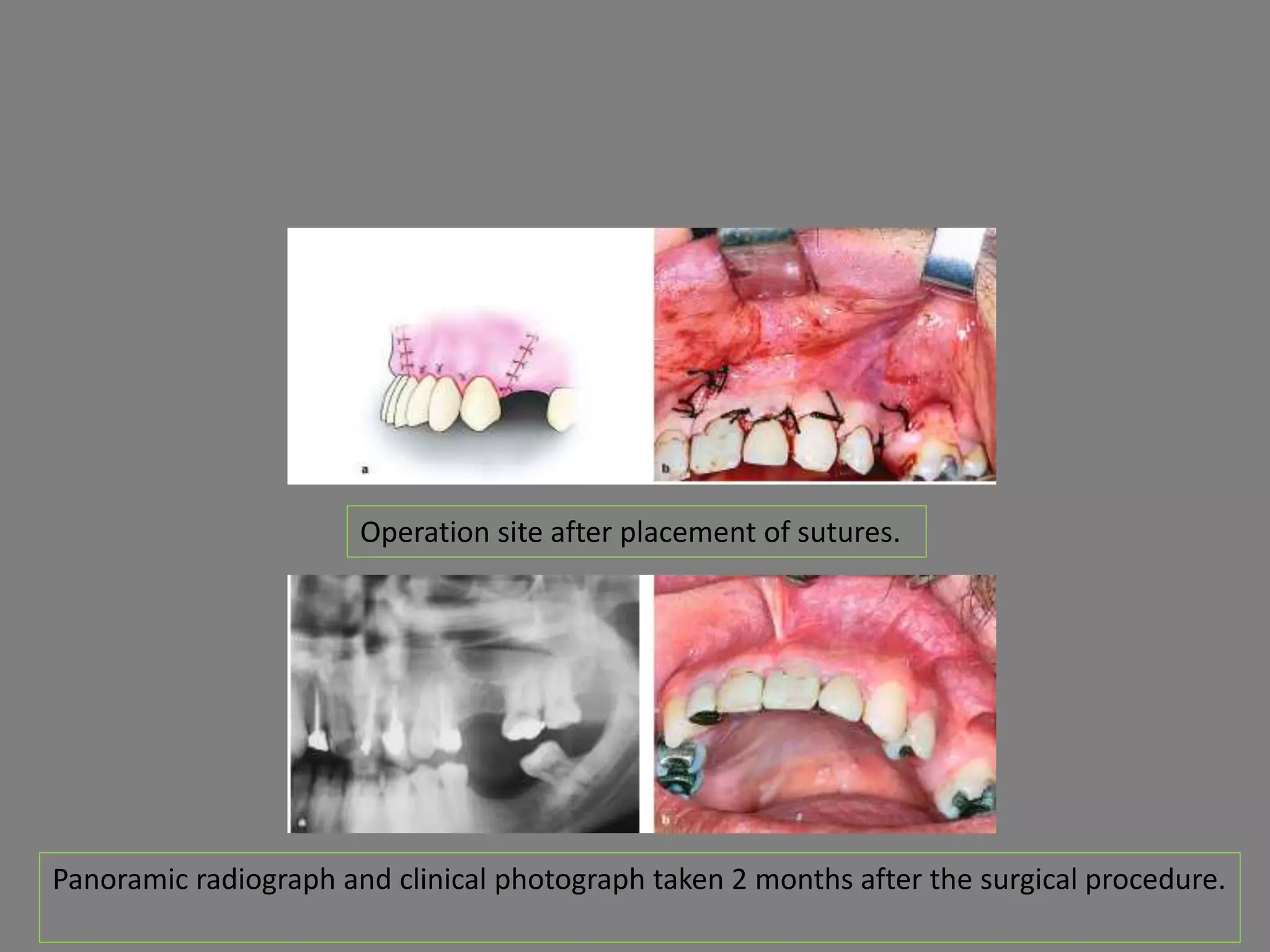
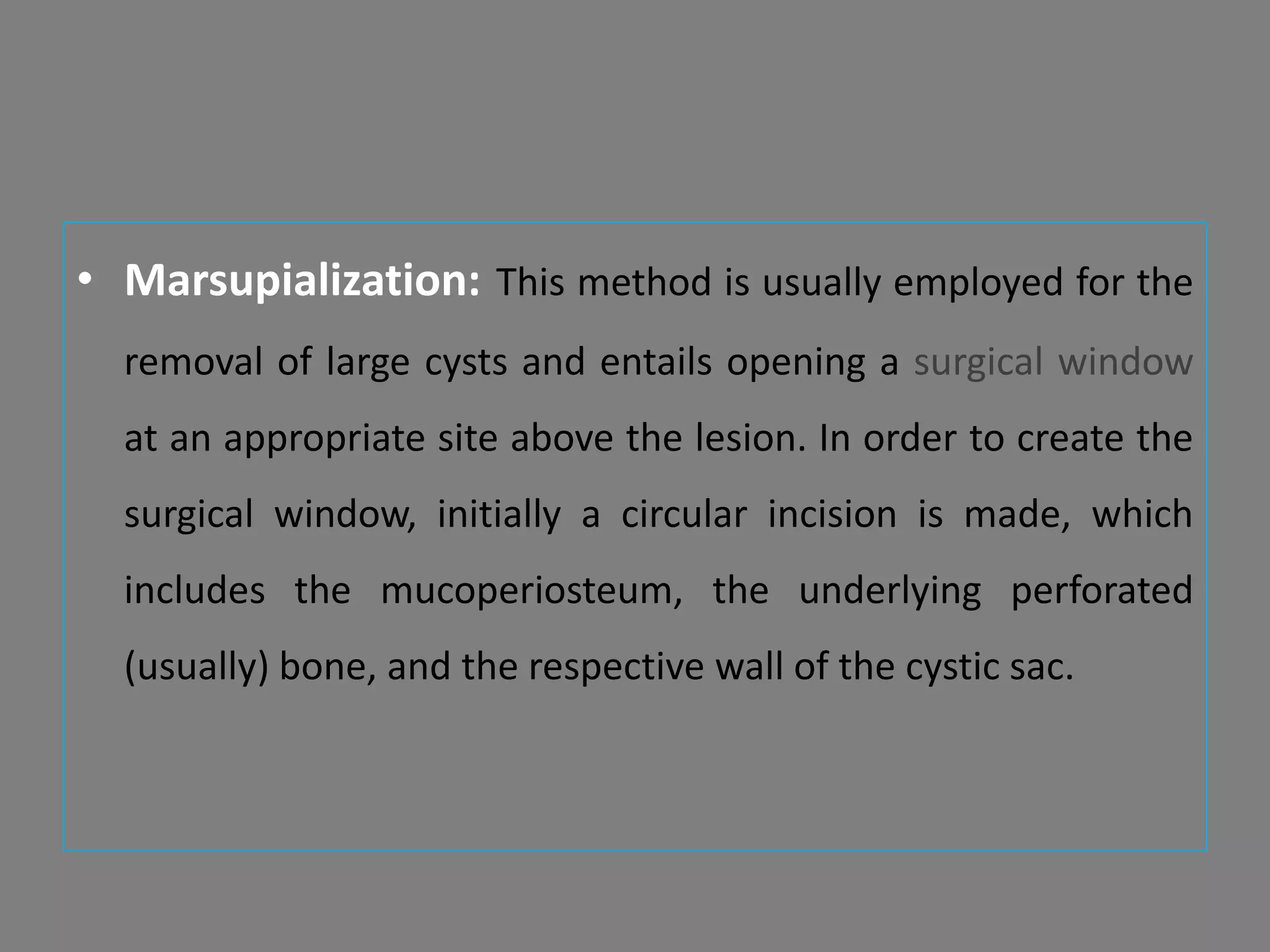
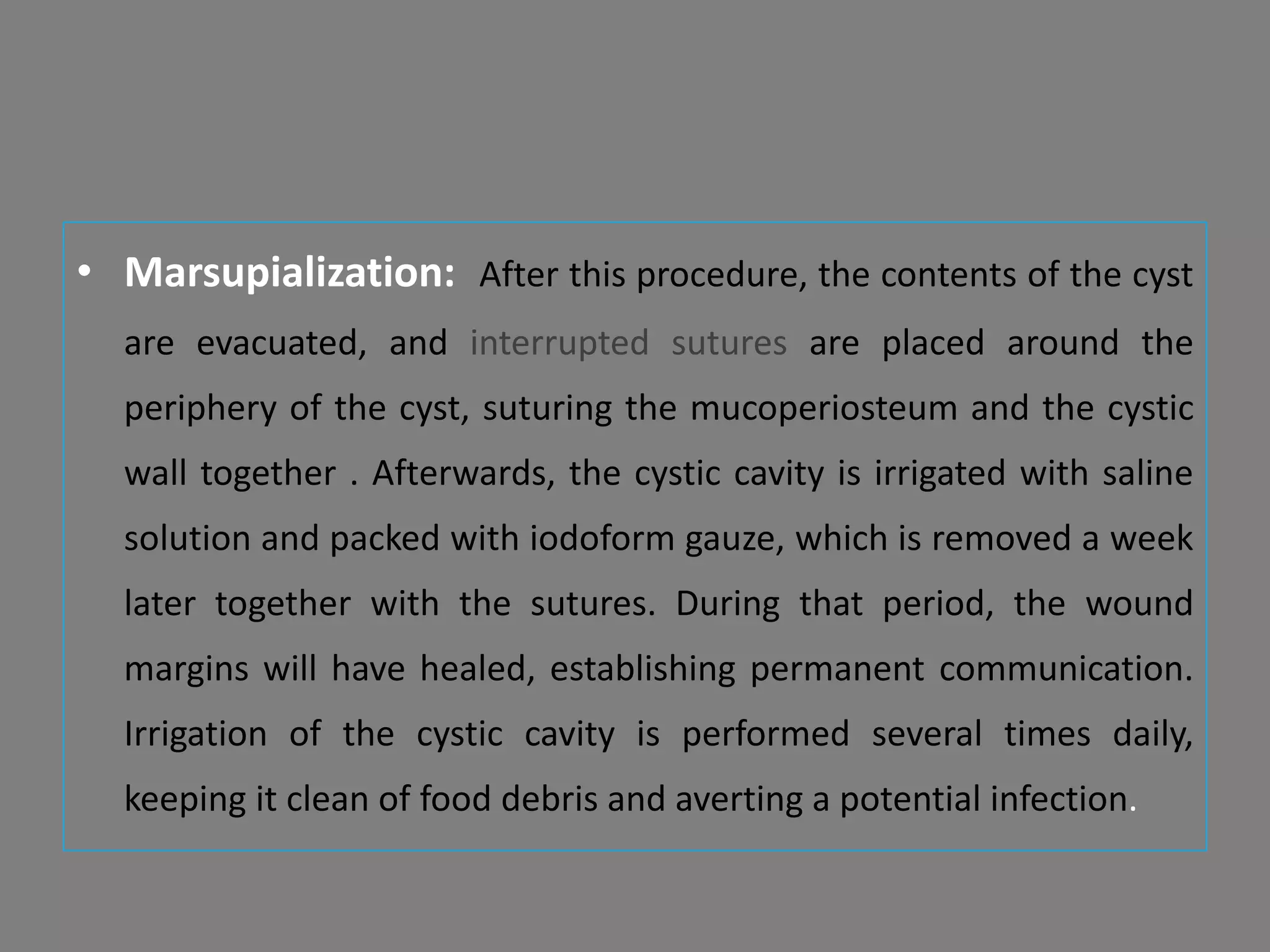
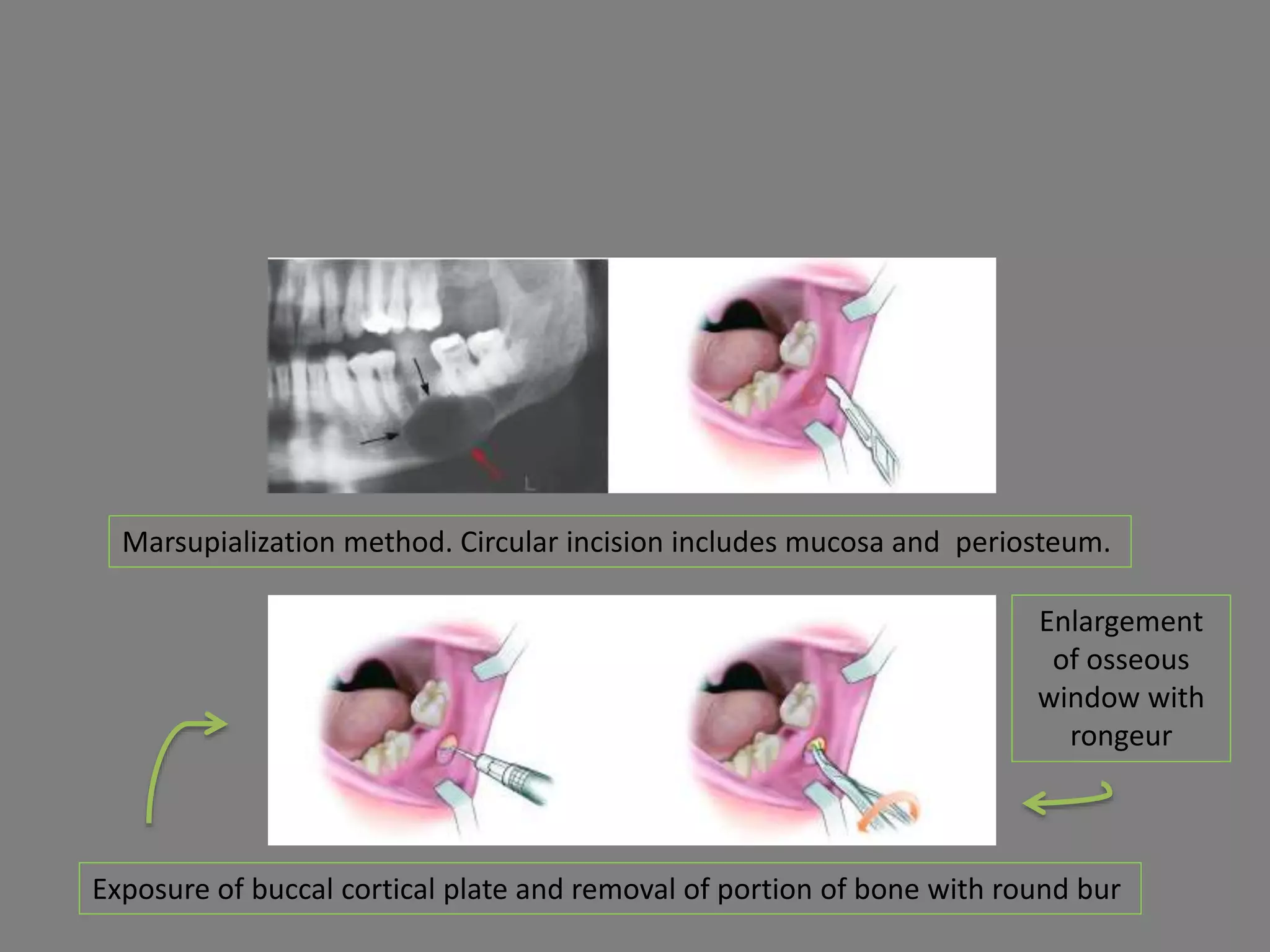
This document discusses odontogenic keratocysts (OKCs), a type of jaw cyst. It covers the classification, causes, histopathology, clinical features, radiographic features, differential diagnosis, treatment principles, and surgical treatment options for OKCs. OKCs most commonly occur in the mandibular molar and ramus areas and are often radiolucent and multilocular in appearance on radiographs. Treatment options include wide surgical excision or marsupialization to prevent recurrence of these cysts which have a high rate of recurrence compared to other jaw cysts.