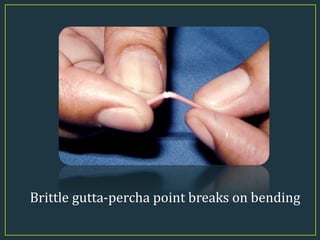
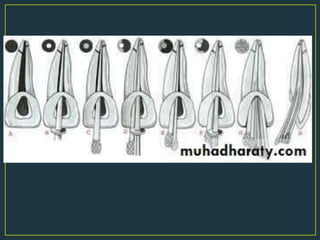
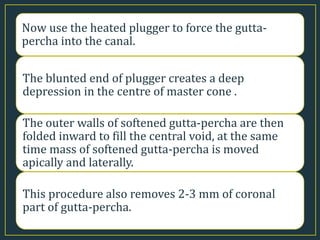
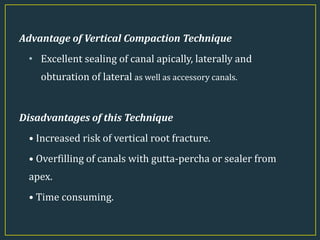
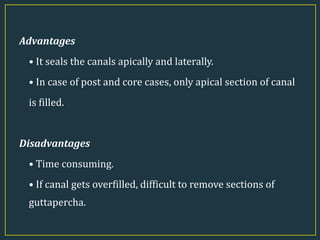
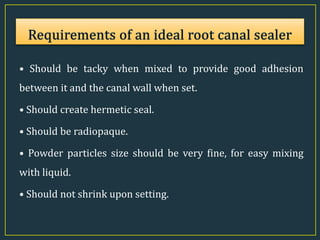
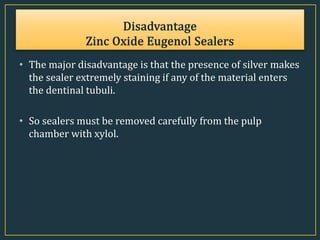
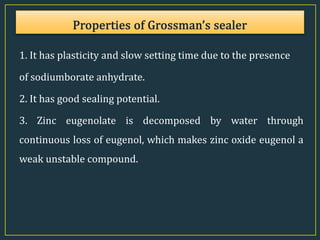
This document discusses different techniques for root canal obturation using gutta-percha. It describes lateral compaction technique which involves using a master gutta-percha cone coated with sealer followed by accessory cones compacted laterally using spreaders. It also describes vertical compaction technique involving softening gutta-percha segments using heated pluggers to vertically compact it filling the entire canal space. The document provides details on properties, types and advantages and disadvantages of various gutta-percha obturation techniques.