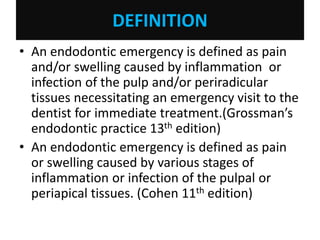
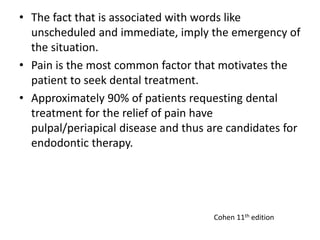
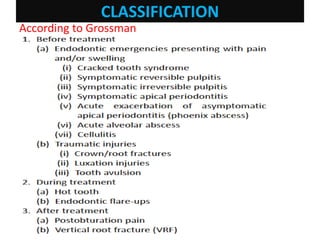
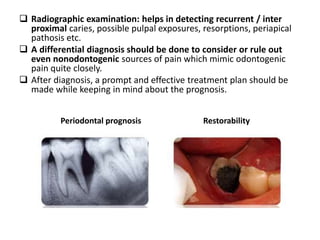
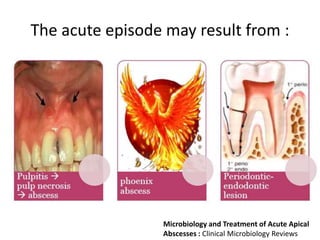
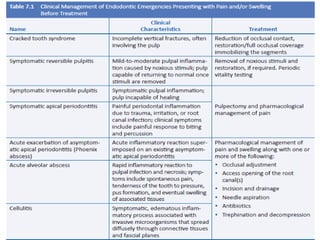
An endodontic emergency is defined as pain and/or swelling caused by inflammation or infection of the pulp and/or periradicular tissues requiring immediate treatment. Common causes are pulpal pathologies and traumatic injuries. Pain results from chemical mediators and increased fluid pressure causing stimulation of pain receptors. Accurate diagnosis involves dental history, clinical examination including vitality testing and radiographs to determine the source and rapidly provide effective treatment.
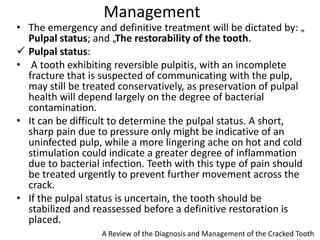
Cracked tooth syndrome is an incomplete fracture of tooth structure causing sharp pain on biting. Risk factors include excessive forces, weakened tooth structure, dental materials or rare events. Symptoms are biting pain and sensitivity. Diagnosis involves visual inspection, transillumination, dyes or bands to detect the crack








![ Apical extrusion of debris:
• Extrusion of infected debris to the periradicular tissues
during chemomechanical preparation is one of the
principal causes of postoperative pain.
• Forcing microorganisms and their products into the
periradicular tissues can generate an acute
inflammatory response, the intensity of which will
depend on the quantitative (number) and qualitative
(virulence) nature of the extruded microorganisms.
• Iatrogenic overinstrumentation promotes the
enlargement of apical foramen, which may permit an
increased influx of exudate and blood into the root
canal.[18] This will enhance the nutrient supply to the
remaining bacteria within the root canal, which can
then proliferate and cause exacerbation of a chronic
periradicular lesion.
Journal of Pharmacy and Bioallied Sciences Vol 4 August 2012
Supplement 2 - Part 3; Harikaran, et al.: Flare-up review](https://image.slidesharecdn.com/endodonticemergenciesdr-210909105225/85/ENDODONTIC-EMERGENCIES-96-320.jpg)