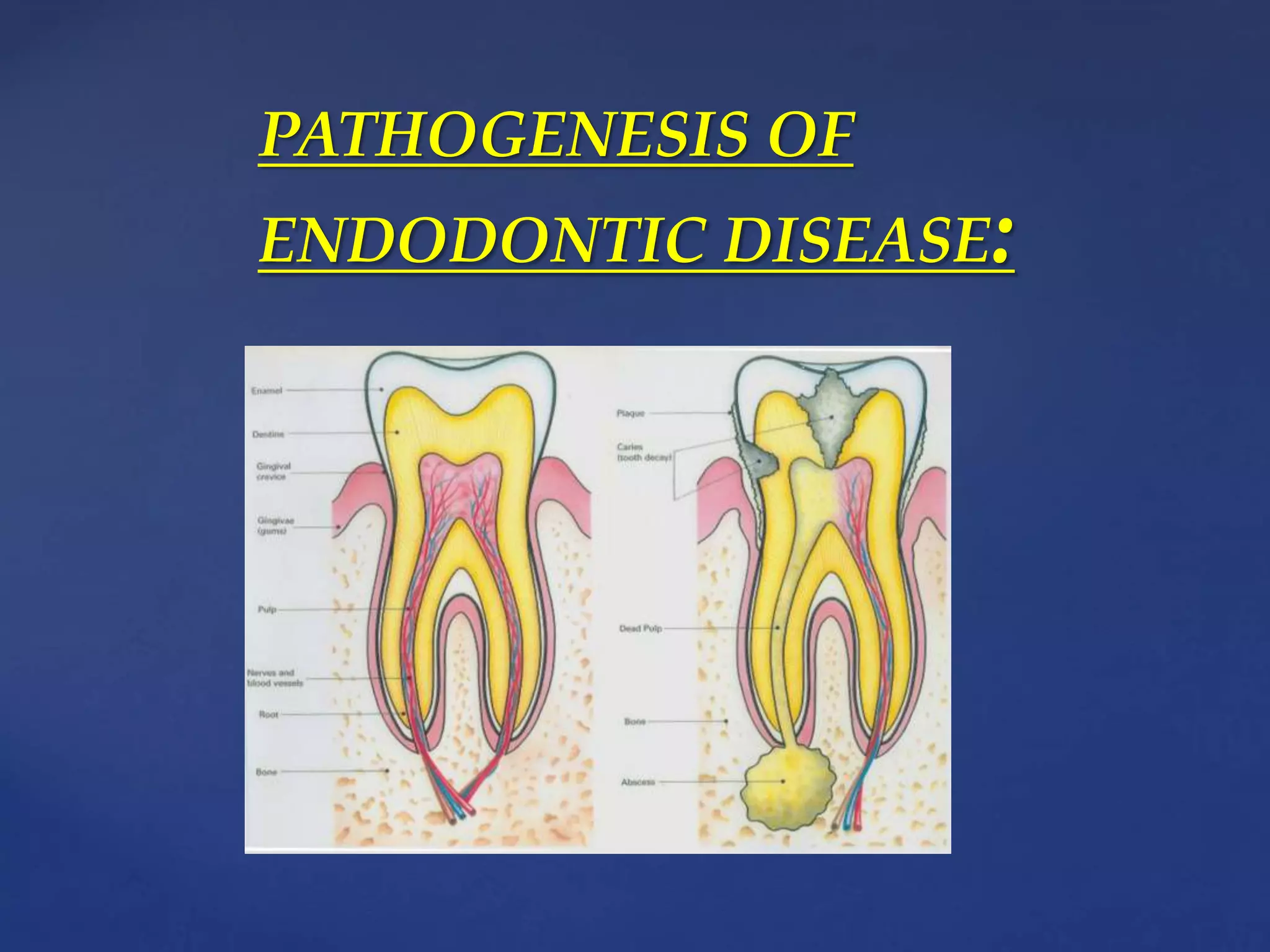
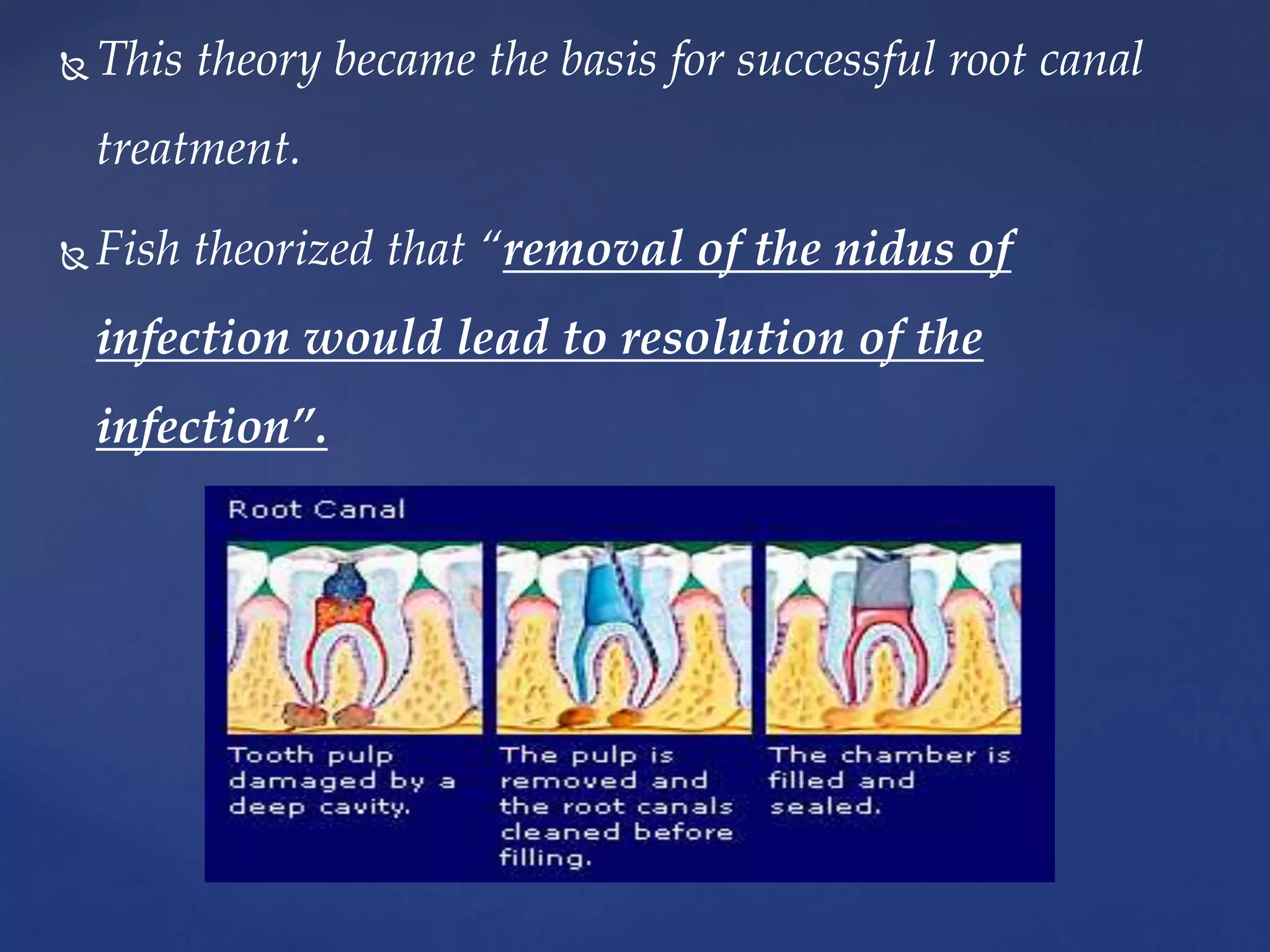
This document provides an overview of endodontics. It defines endodontics as the branch of dentistry concerned with the morphology, physiology, and pathology of the dental pulp and periradicular tissues. The scope of endodontics includes treating diseases of the pulp, such as pulpal inflammation and infection, through both nonsurgical and surgical root canal treatment and periradicular surgery. Pathogenesis is discussed, noting that while physical and chemical factors can induce inflammation, microbial infection is essential for progression of pulpal and periradicular disease. Routes of canal infection and the focal infection theory are also summarized.




















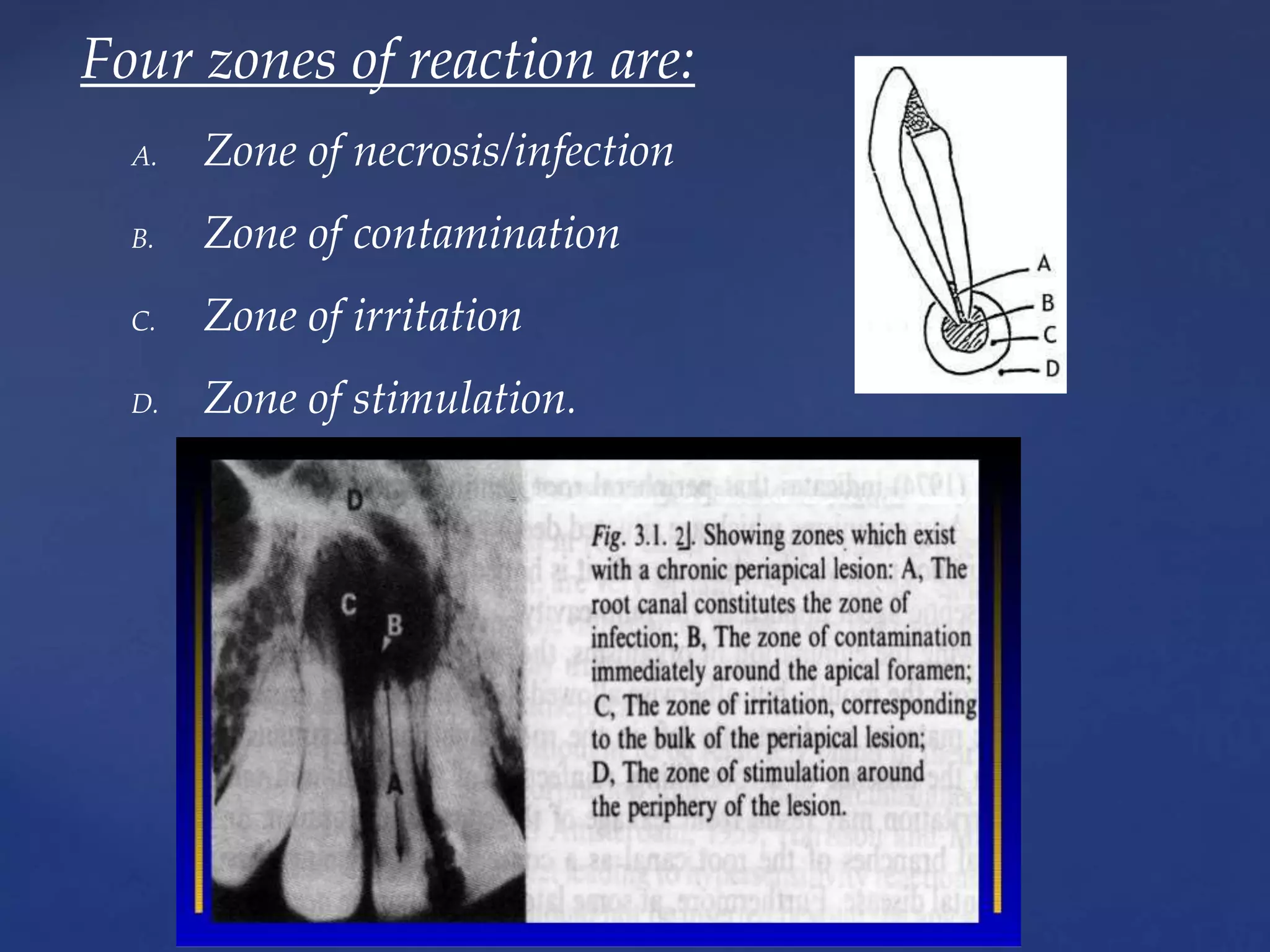




![ Zone A:
• He compared the bacteria in the infected root canal with
the invaders entrenched behind high and inaccessible
mountain pass.
Zone B:
• The exudative and granulomatous tissue of the
granuloma represents a mobilized army defending the
plains[periapex] from the invaders [bacteria]
• When a few microbes enter the periapex, they are
destroyed by PMNs.](https://image.slidesharecdn.com/1rationaleofendodontics17thnov1456-180923150251/75/Rationale-of-endodontics-47-2048.jpg)

![ Zone C:
• Only complete elimination of the invaders from their
mountainous entrenchment will eliminate the need of
a defence forces in the “plains”.
• Once this is accomplished, the defending army of
leukocytes withdraws, the local destruction created by
the battle is repaired [granulation tissue] and the
environment results to normal.](https://image.slidesharecdn.com/1rationaleofendodontics17thnov1456-180923150251/75/Rationale-of-endodontics-49-2048.jpg)