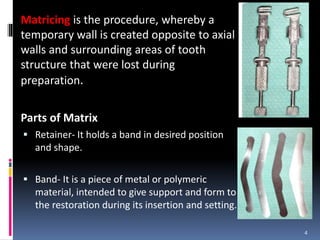
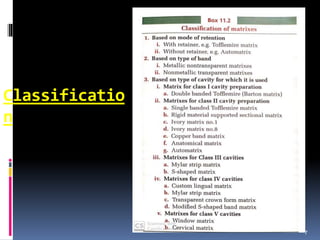
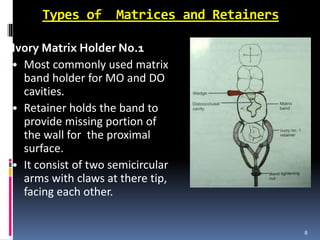
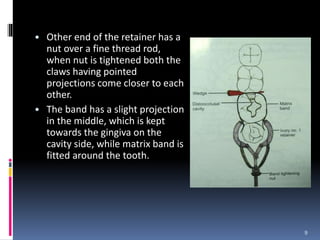
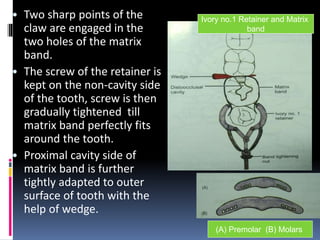
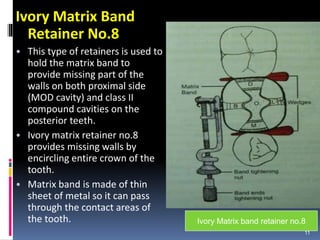
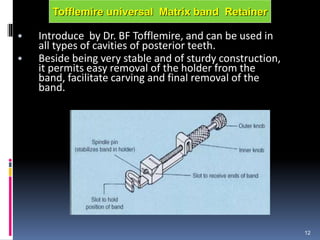
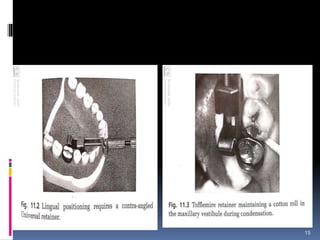
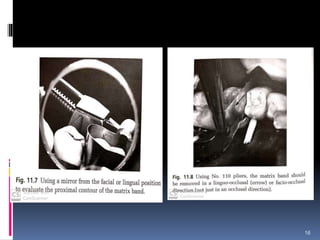
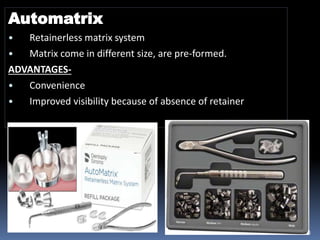
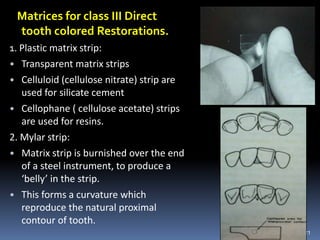
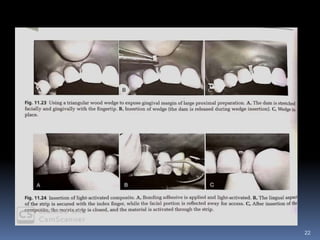
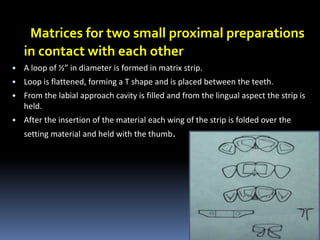
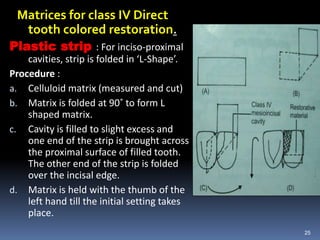
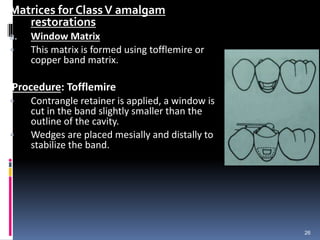
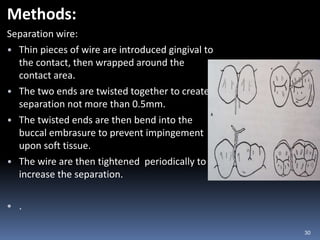
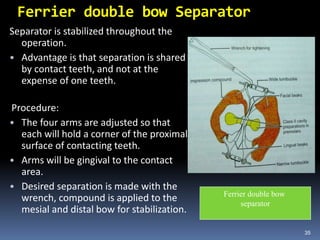
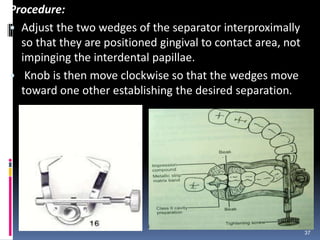
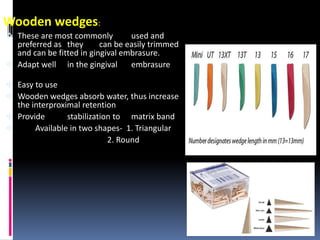
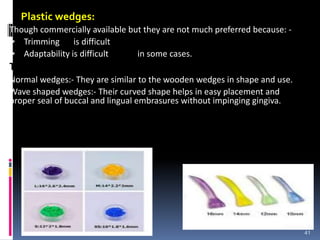
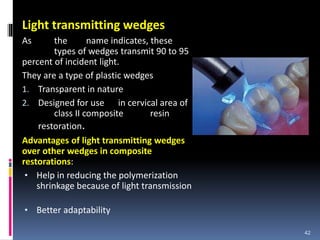
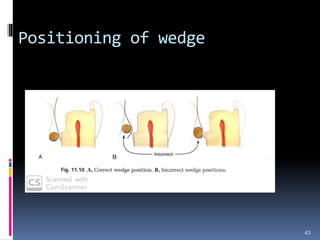
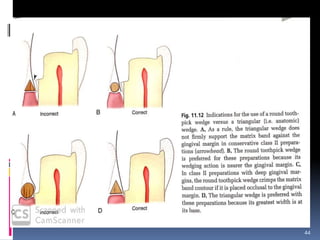
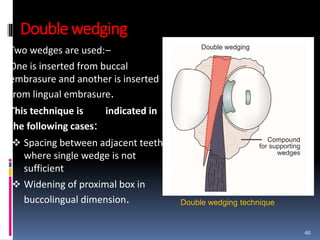
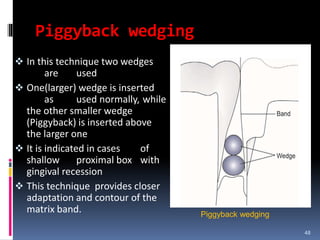
The document discusses dental matrices, wedges, and separators, detailing their definitions, ideal requirements, types, and recent advancements. It emphasizes the importance of matrices in supporting and shaping dental restorations and classifies various matrix systems, including automatrix and traditional devices. The document also addresses wedging techniques and separators for tooth restoration, outlining their functions and specific methods used in dental procedures.