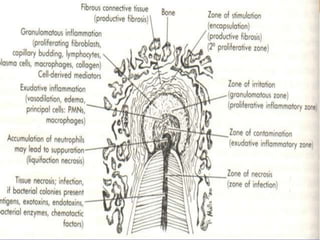
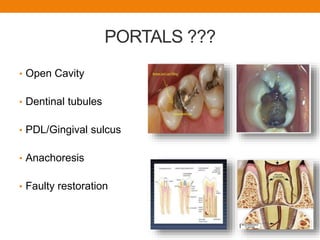
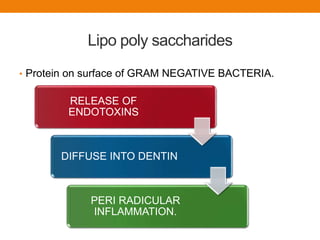
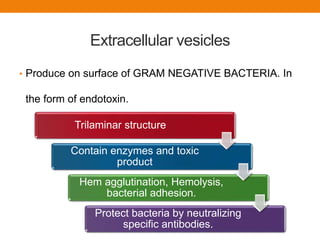
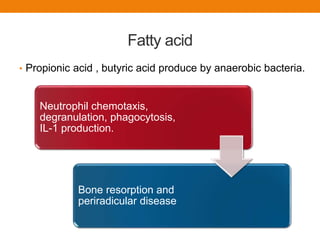
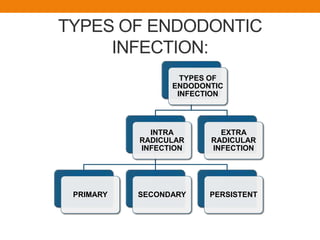
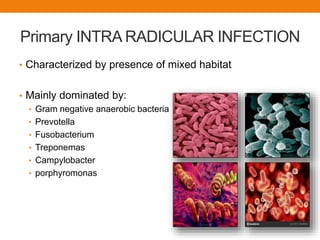
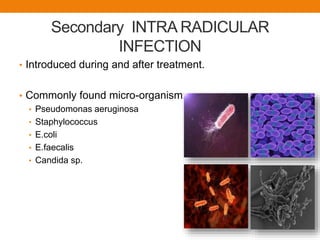
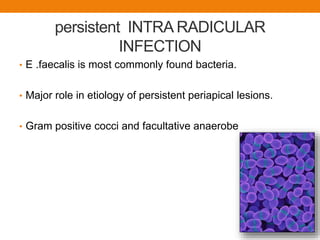
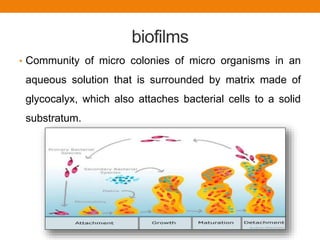
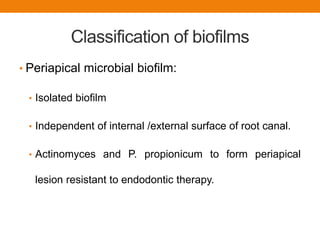
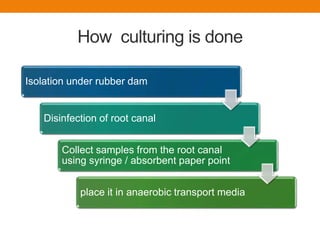
This document discusses endodontic microbiology. It begins by explaining the importance of effective diagnosis and treatment of endodontic infections. It then discusses the various portals of entry for microorganisms into the root canal system. The document classifies bacteria found in endodontic infections and discusses their pathogenicity and virulence factors. It describes the different types of intra-radicular and extra-radicular infections and highlights Enterococcus faecalis as the bacteria most commonly associated with persistent infections. The final sections discuss biofilms in endodontic infections and methods to identify bacteria through culture, Gram staining, and molecular diagnostic techniques like DNA-DNA hybridization and polymerase chain reaction.