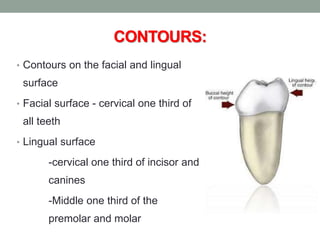
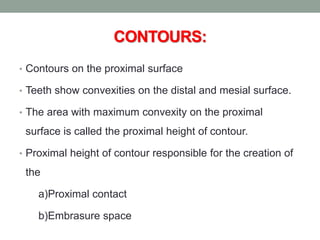
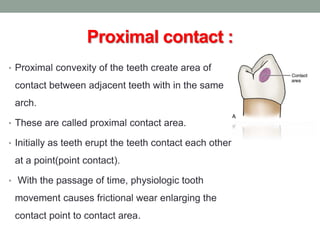
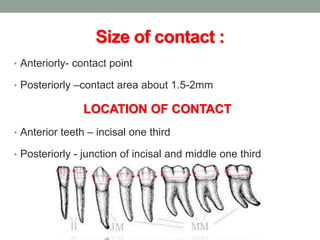
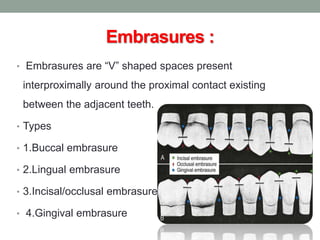
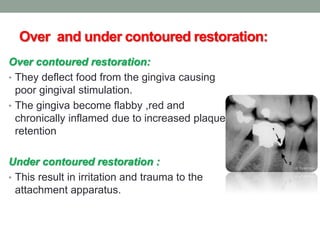
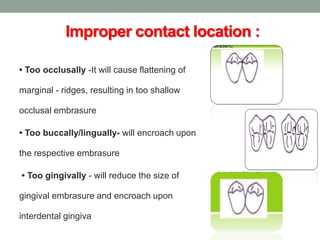
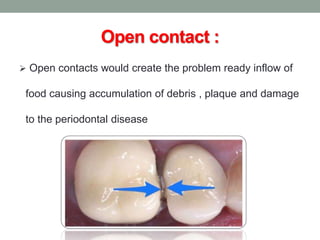
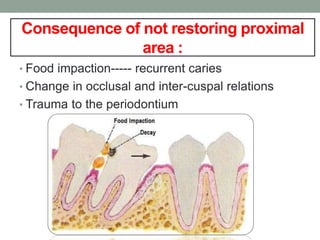
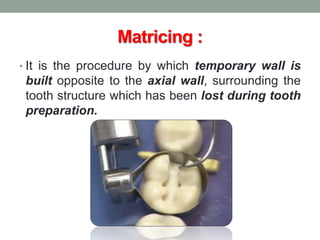
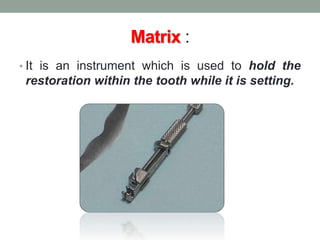
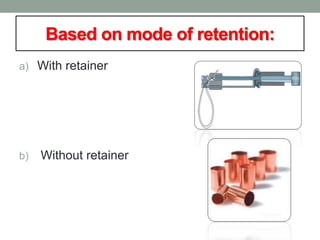
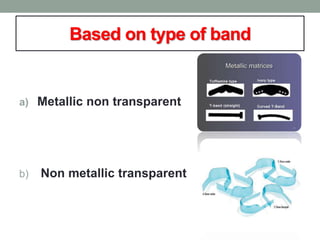
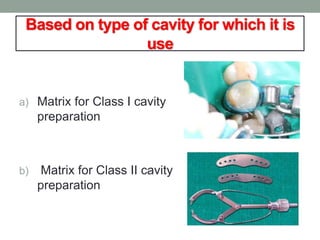
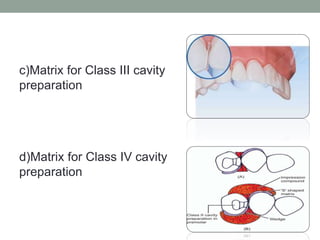
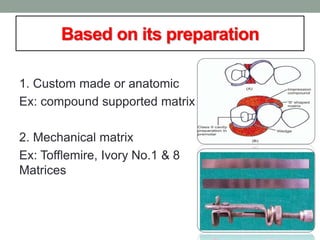
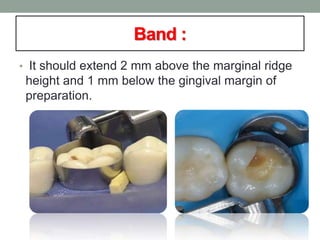
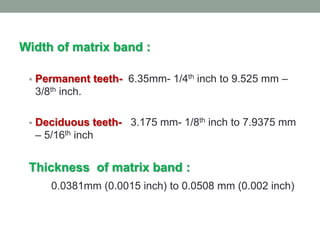
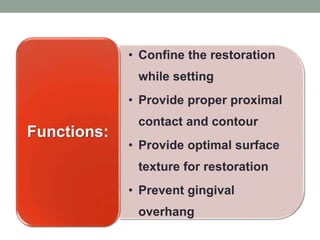
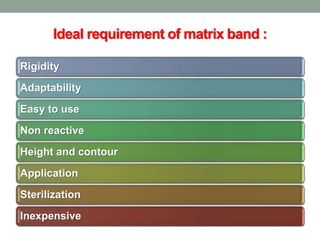
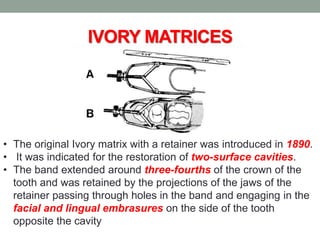
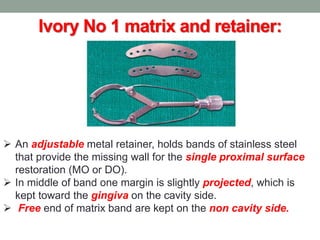
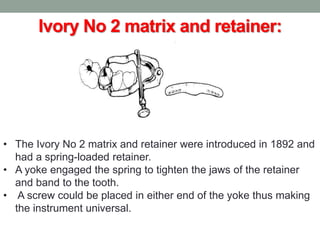
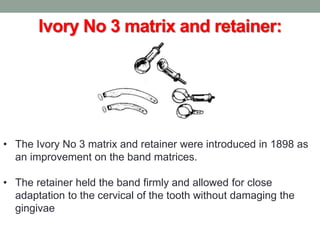
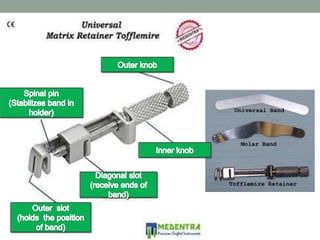
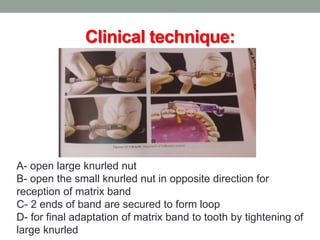
This document discusses dental contours and tooth separation. It describes the different contours on facial, lingual, proximal, and occlusal surfaces. Proper proximal contacts and embrasure spaces are important for stability, preventing food impaction, and protecting soft tissues. Matrices are used to form contacts and contours during restorative procedures. Various matrix systems and methods of tooth separation like wedges and separators are outlined. Maintaining ideal contacts, contours, and embrasure sizes is important for function and periodontal health.