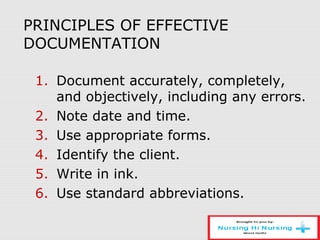
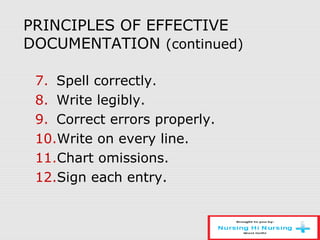
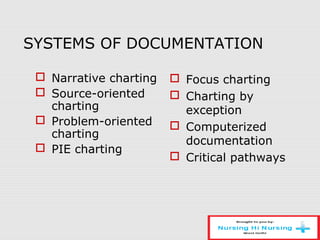
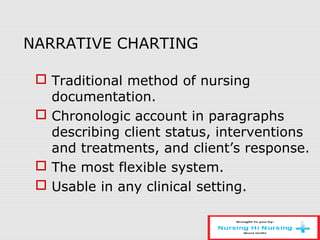
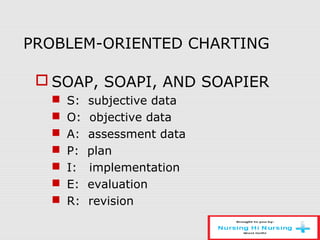
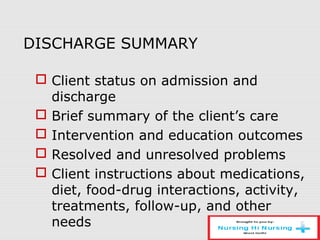
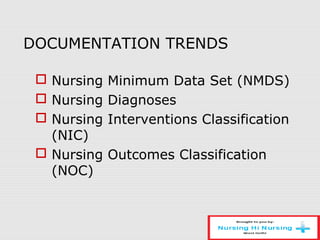
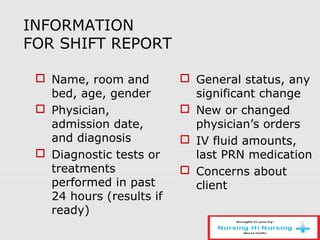
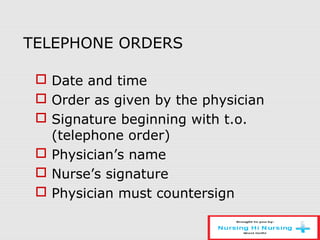
The document discusses the nursing process and documentation. It describes the 5 steps of the nursing process as assessment, diagnosis, planning, implementation, and evaluation. It then explains each step in detail including types of assessments, sources of data, nursing diagnoses, care planning, interventions, and evaluation. The document also discusses principles of documentation, various documentation systems, and specific documentation tools like progress notes and discharge summaries.