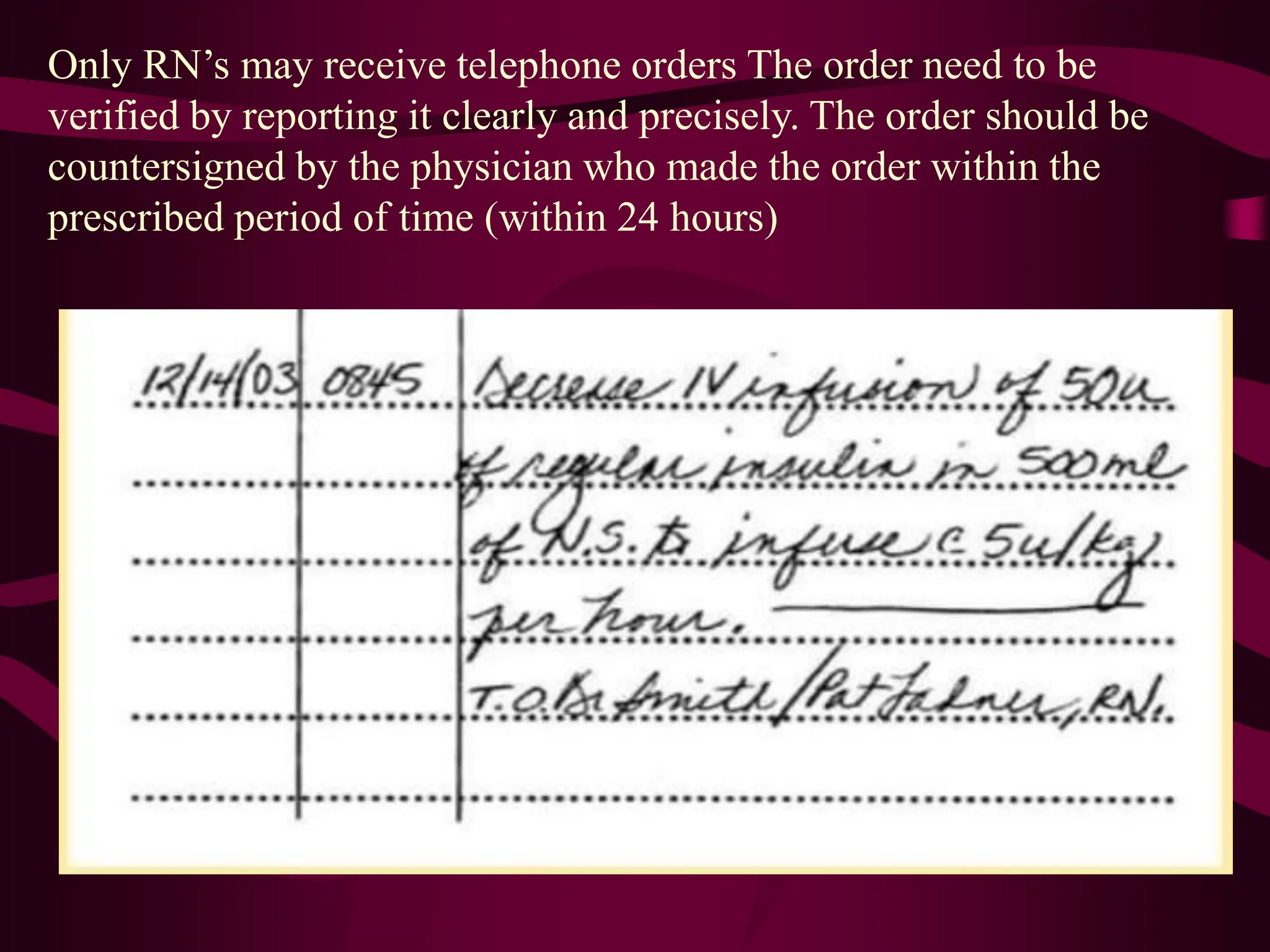
The document outlines the importance of documentation and reporting in healthcare, emphasizing its role in communication, legal evidence, research, and care planning. It details the components and types of medical records, effective documentation practices, and various methods for recording and reporting patient information. Additionally, it provides guidelines for maintaining accuracy, confidentiality, and compliance in documentation to enhance patient care and minimize legal liability.