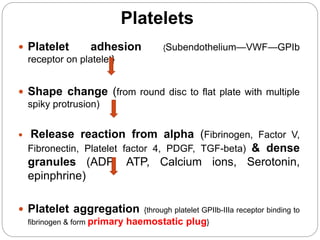
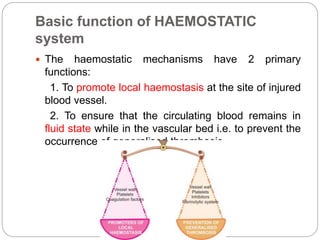
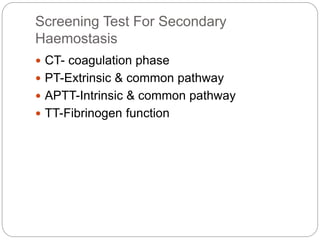
This document discusses haemostasis, the process by which bleeding is stopped. It describes the key components of the haemostatic system, including platelets, coagulation factors, and the endothelium. The sequence of events that occurs at the site of vascular injury is outlined, from initial platelet plug formation to stabilization of the fibrin clot. The roles of platelets, coagulation factors, fibrinolysis, and the endothelium are explained. Causes of bleeding disorders include problems with platelets, coagulation factors, fibrinolysis or the endothelium. The document also covers approaches to evaluating bleeding disorders.