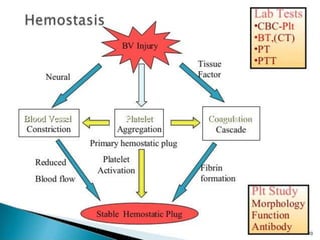
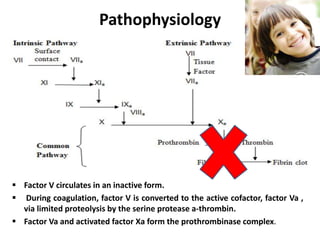
Factor V deficiency, also known as Owren’s disease, is a rare bleeding disorder caused by insufficient or dysfunctional factor V, leading to impaired blood coagulation. It can be inherited (autosomal recessive) or acquired due to immune responses and presents with a range of bleeding symptoms from mild bruising to severe hemorrhaging. Diagnosis is based on laboratory assays showing decreased factor V activity, and treatment involves fresh frozen plasma infusions and monitoring, with no known prevention for the inherited form.

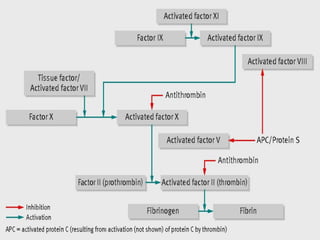



![Laboratory Studies
Factor V assay (decreased activity) .
Bleeding time (prolonged in severe case).
aPTT (Prolonged).
PT (Prolonged).
Thrombin time (Normal).
Stypven time (Russell viper venom time [RVVT]):
(Prolonged).
Correction of PT or partial thromboplastin time
(PTT) with the mixing of equal amounts of normal
and patient plasma.](https://image.slidesharecdn.com/factorvdeficiency-200114180910/85/Factor-v-deficiency-20-320.jpg)