The document provides information on the three lines of defense against microbial pathogens in the human body:
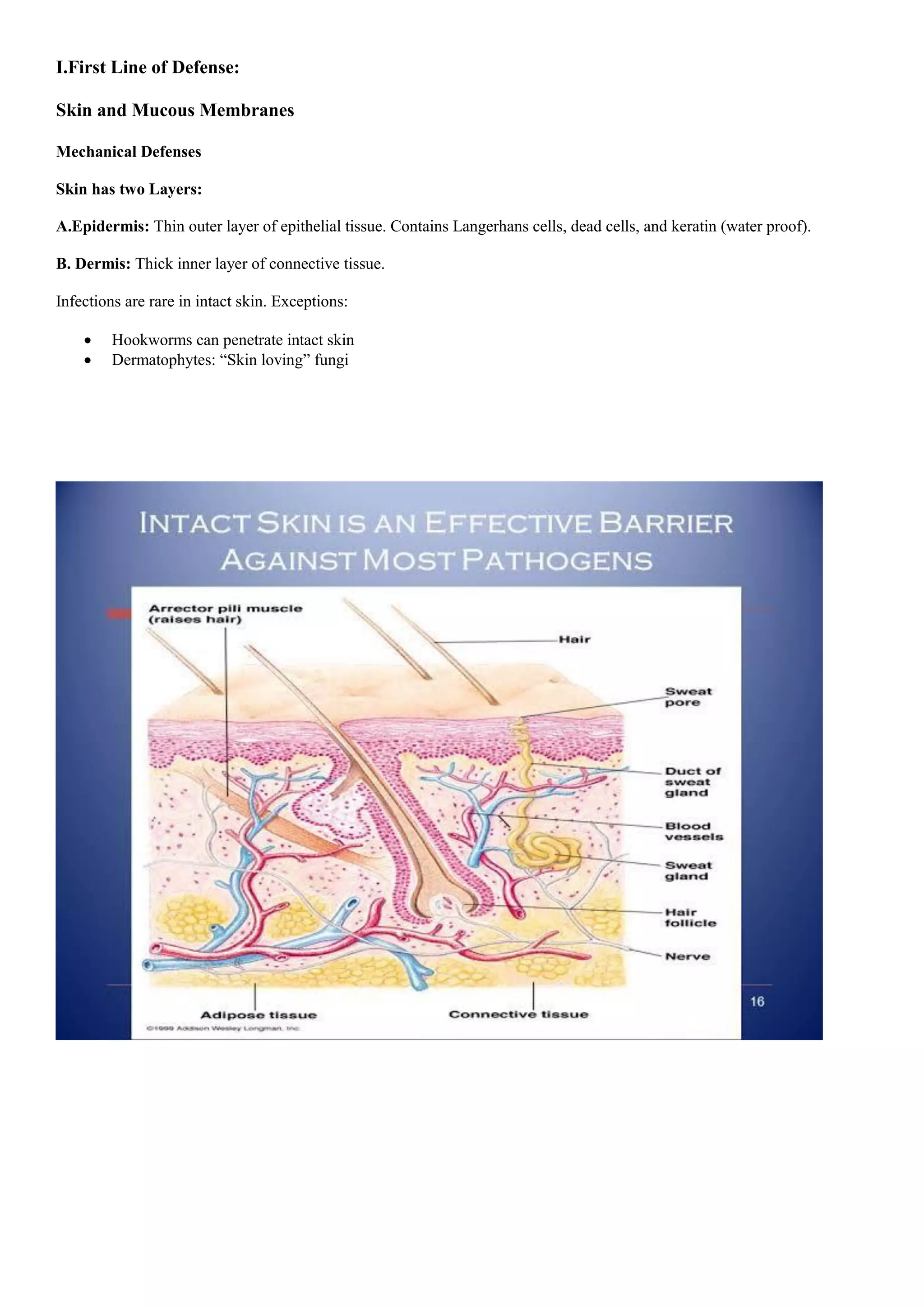
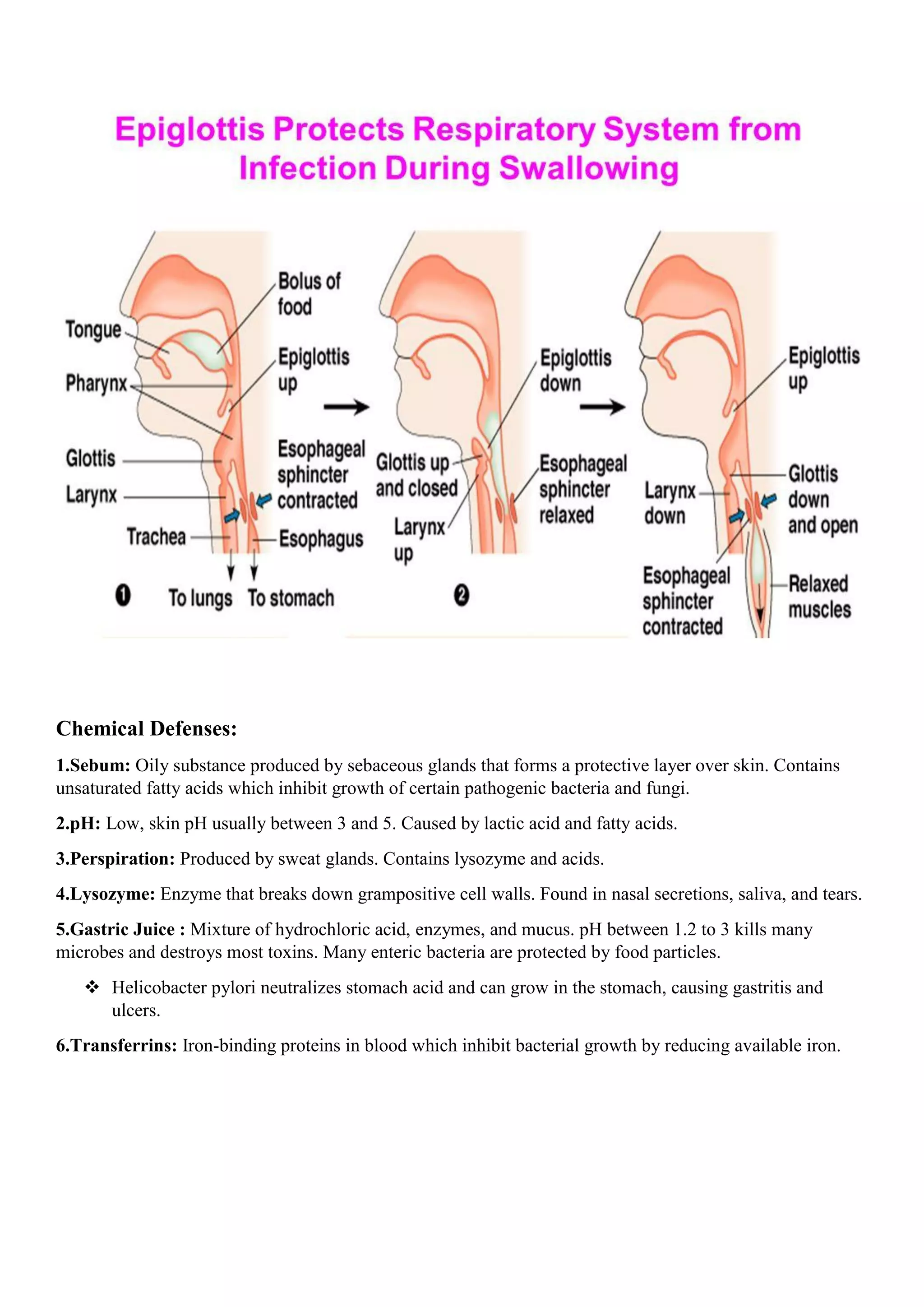
1) The first line of defense consists of natural barriers like intact skin and mucous membranes that prevent pathogen entry.
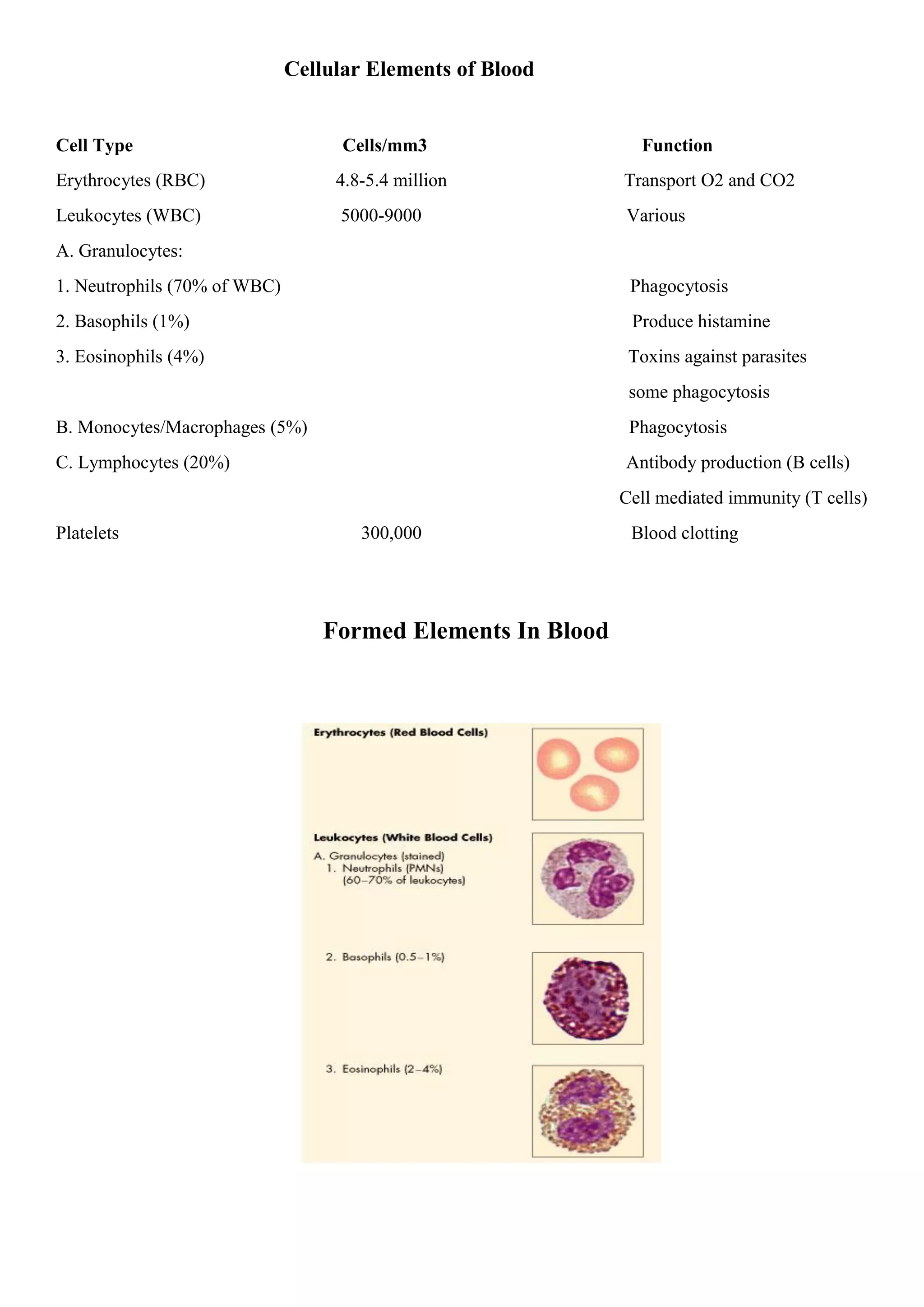
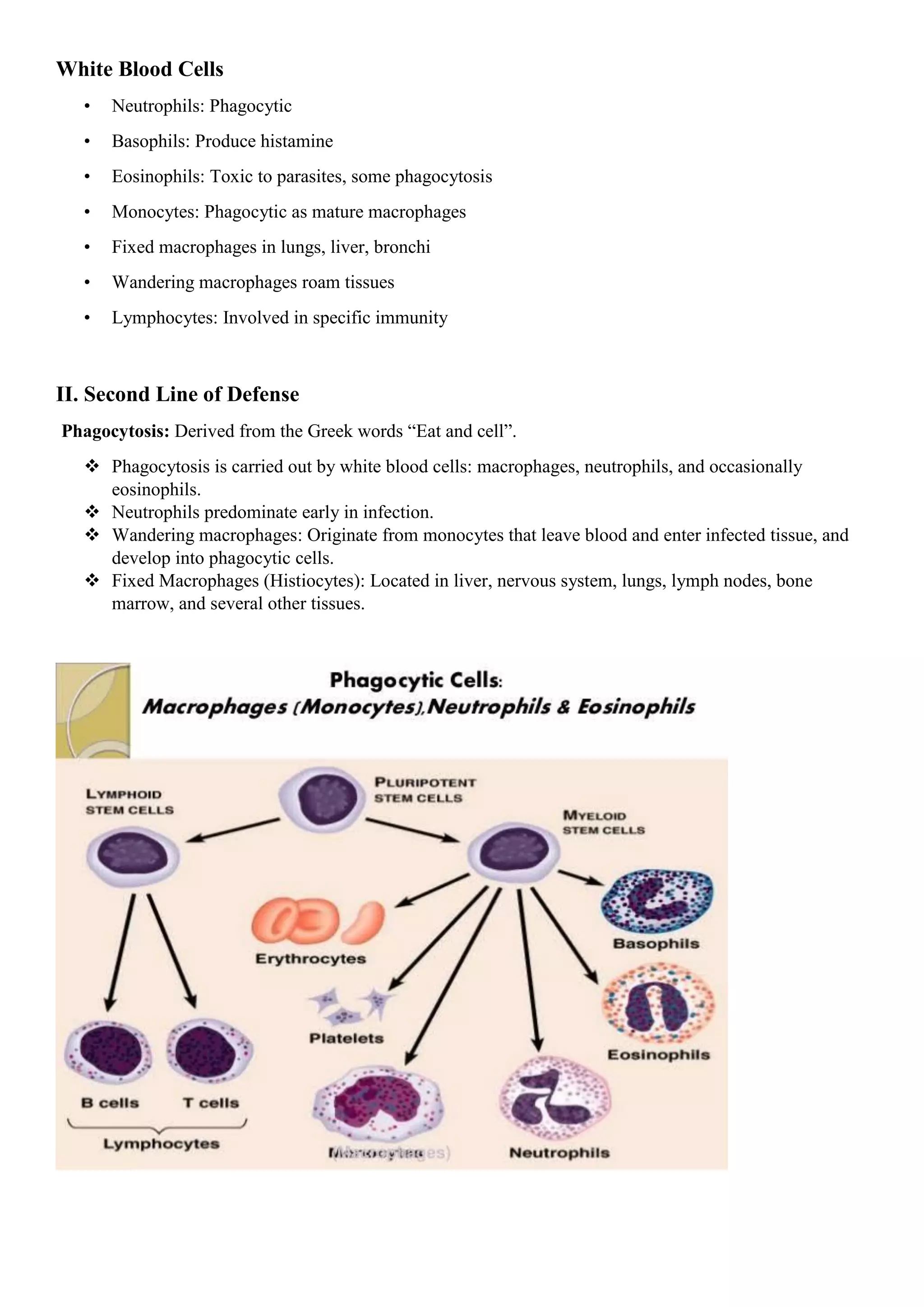
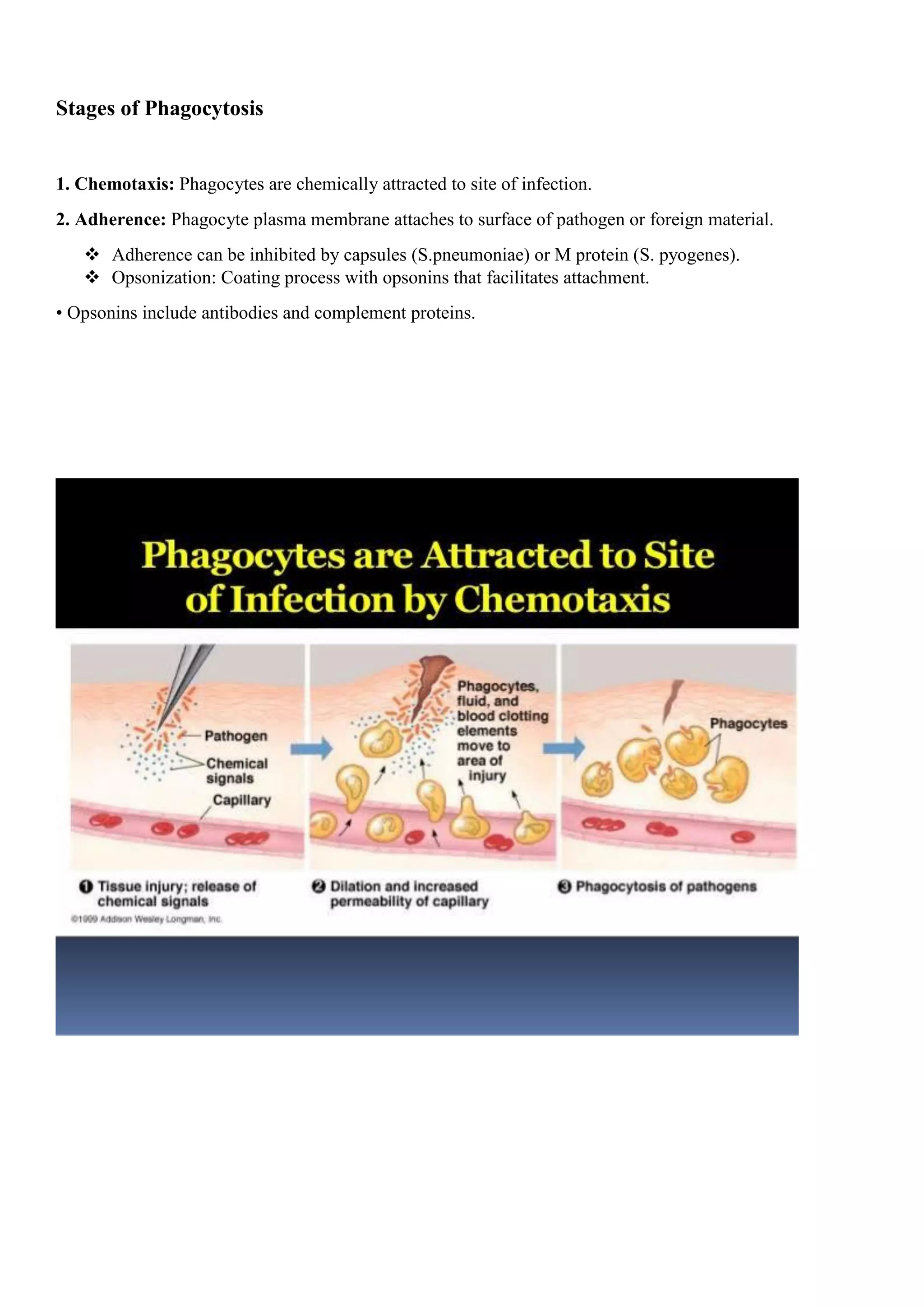
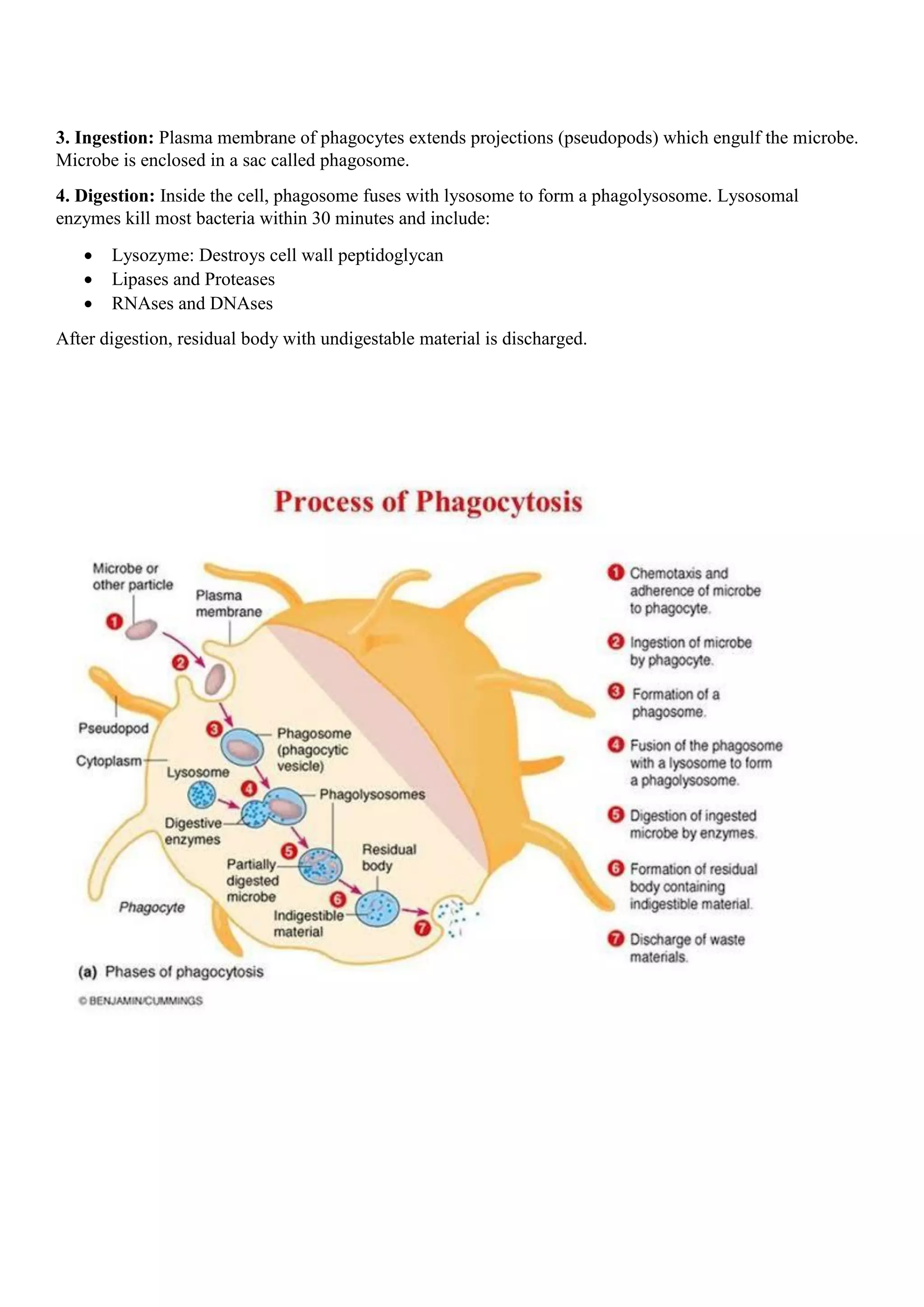
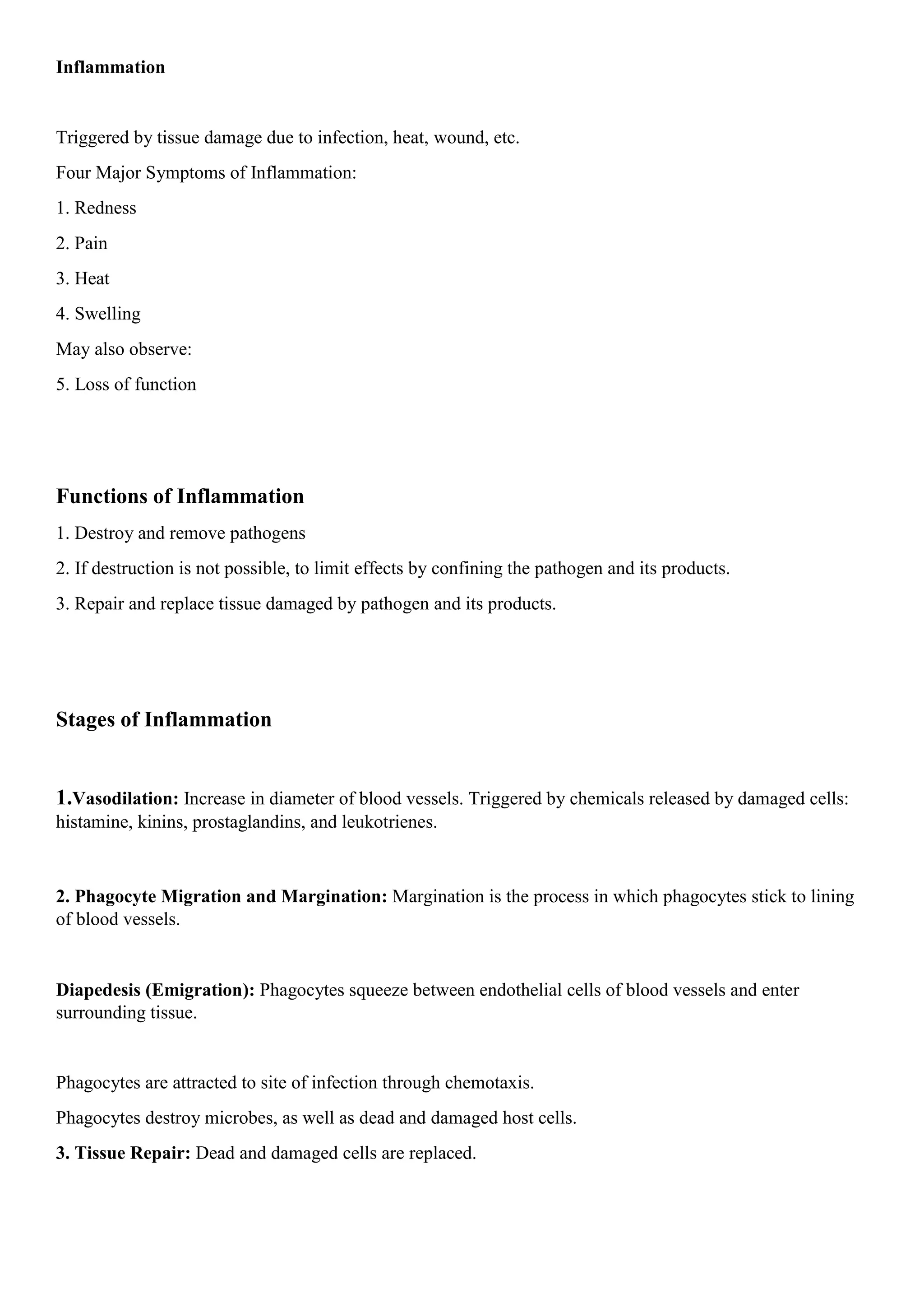
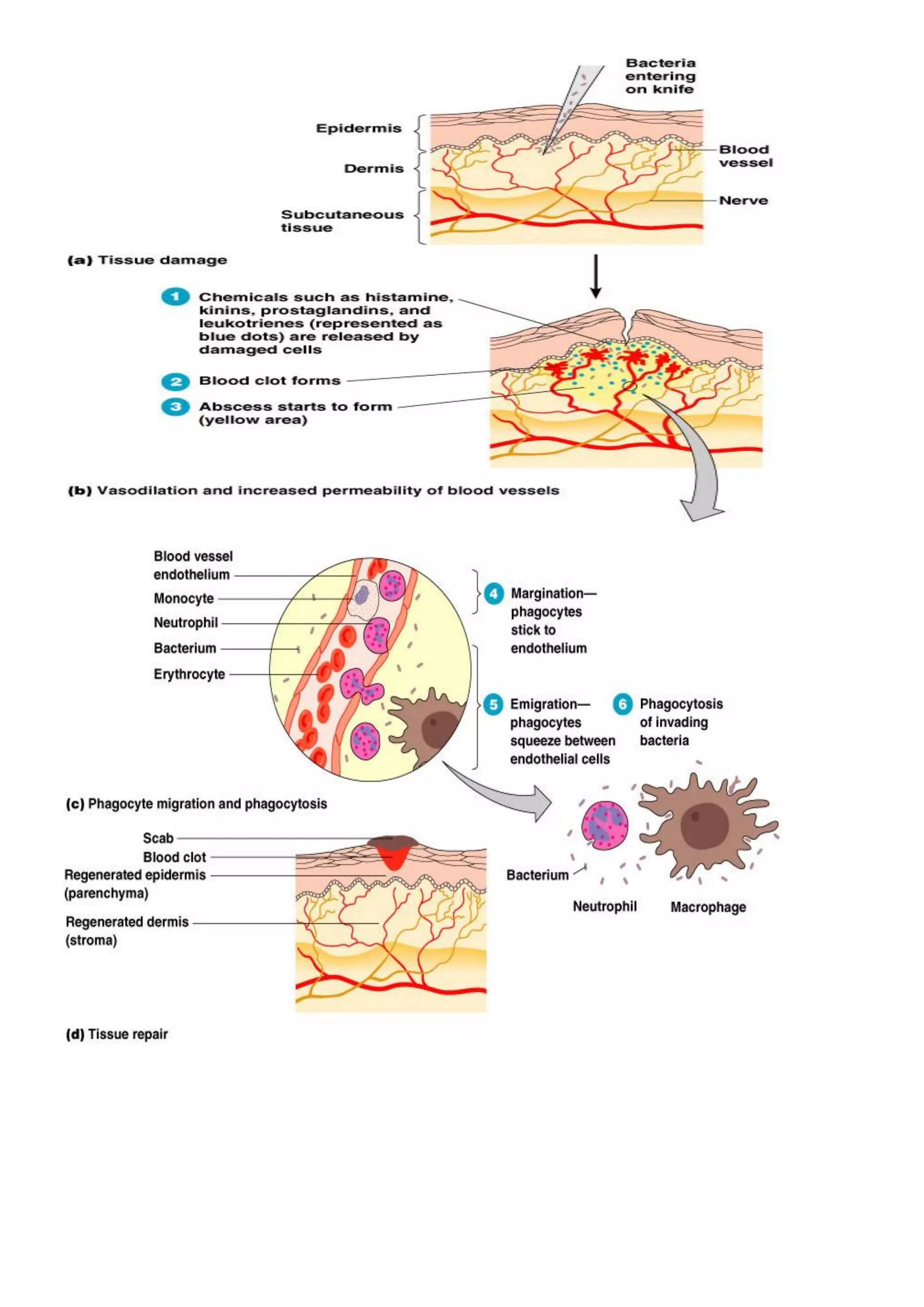
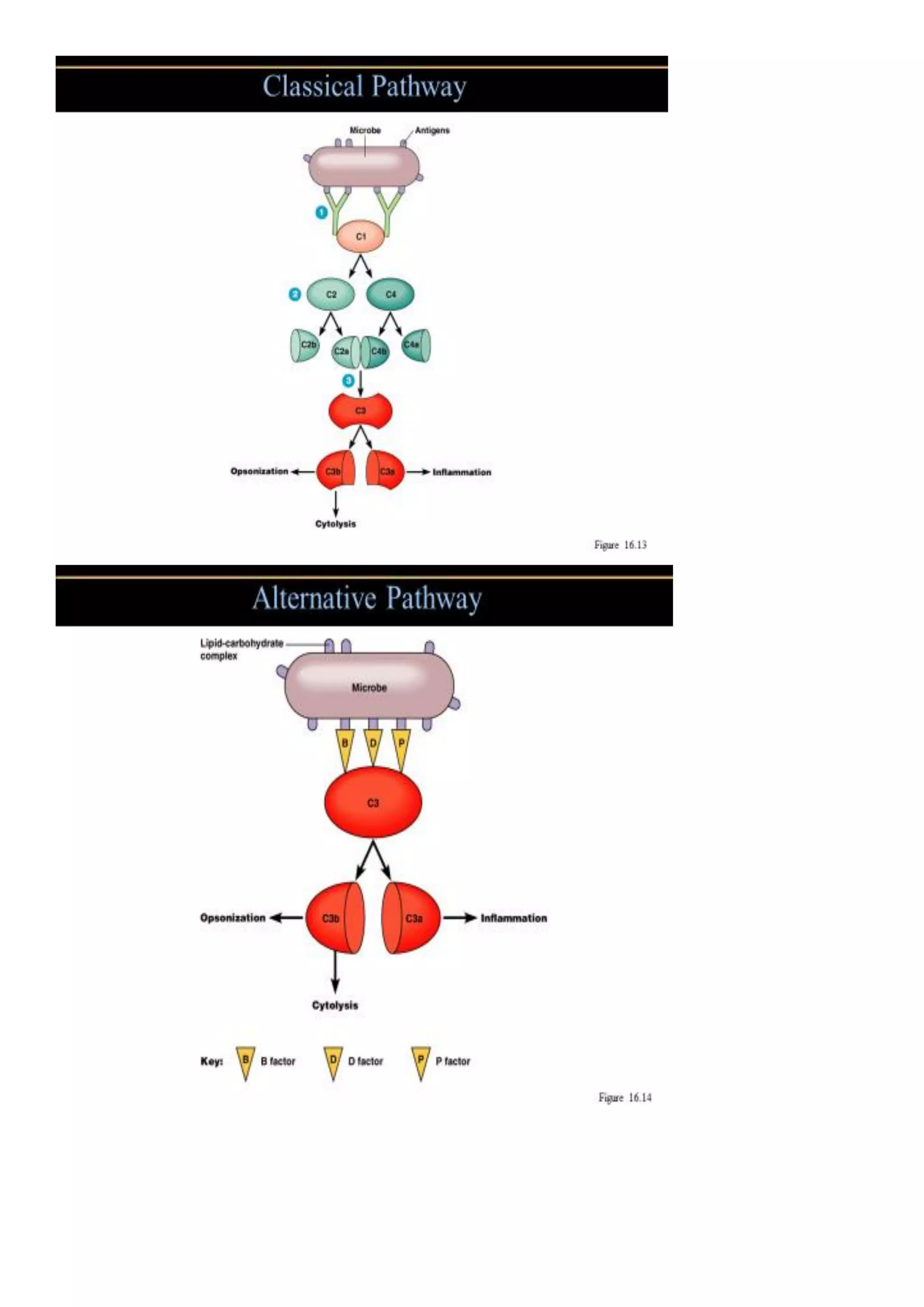
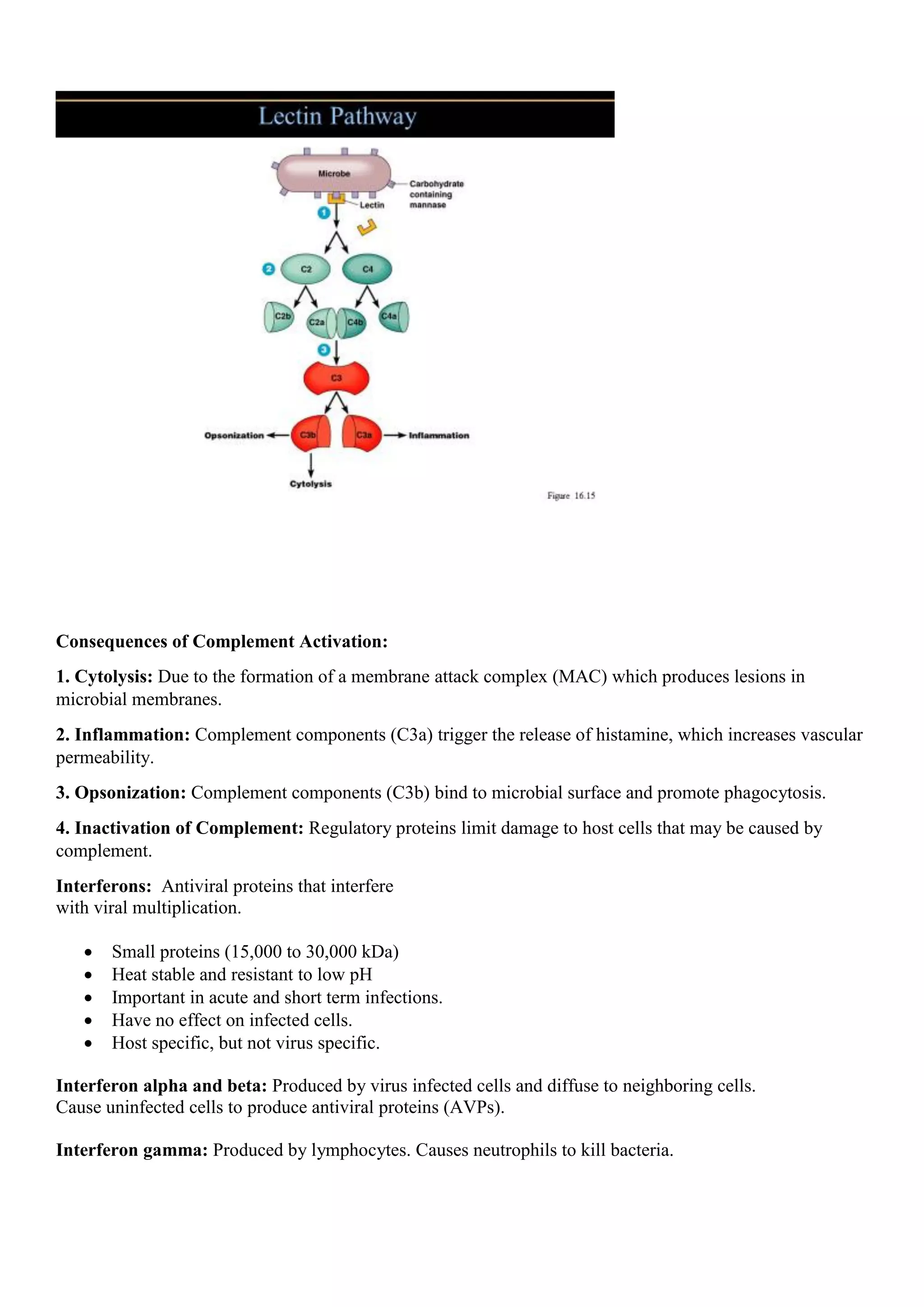
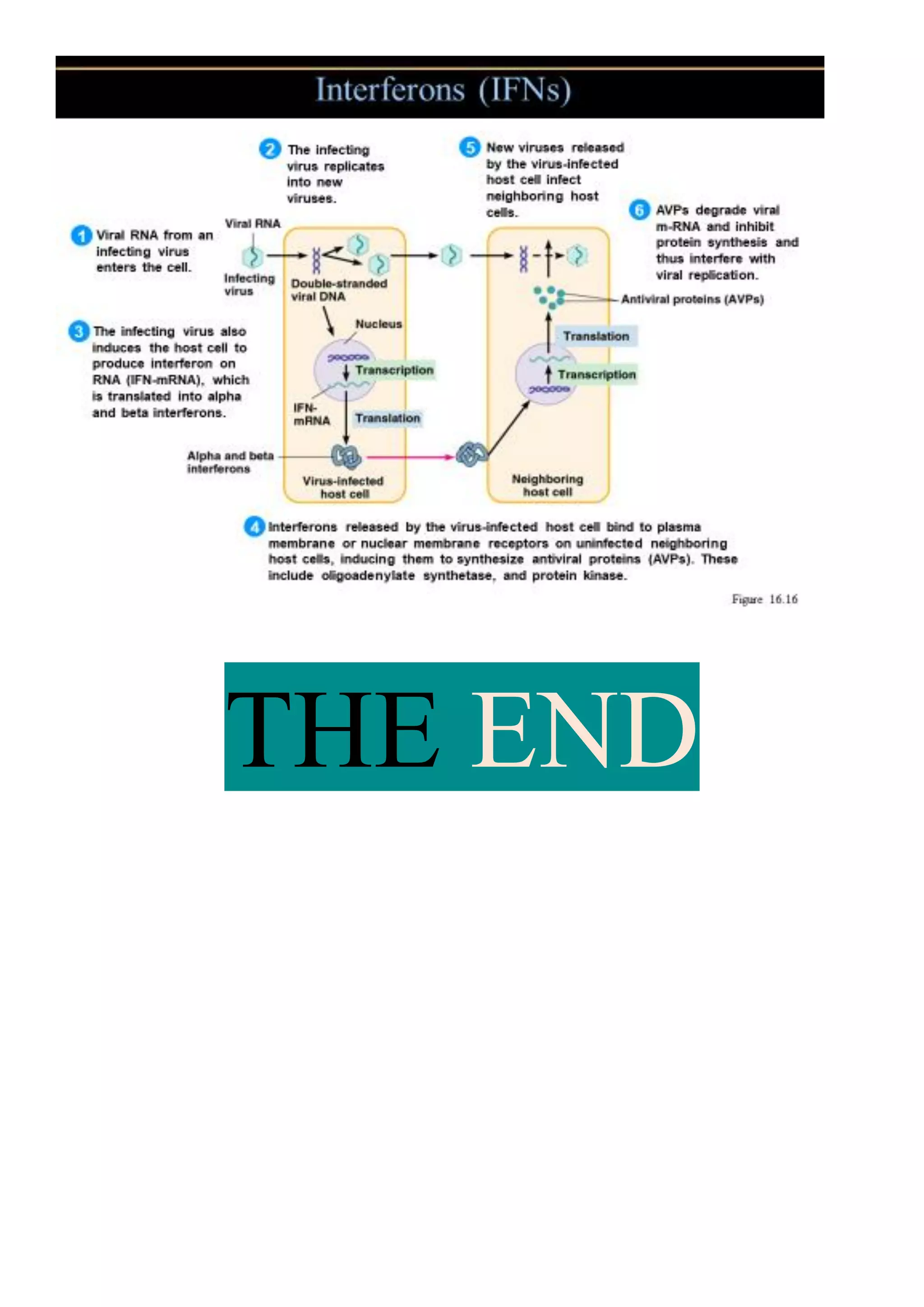
2) The second line of defense involves innate immune responses after pathogen entry, such as phagocytosis by white blood cells, inflammation, and antimicrobial substances like the complement system and interferons.
3) The third line of defense consists of antigen-specific adaptive immune responses mediated by lymphocytes and antibodies that specifically target pathogens that breach the first two lines of defense.