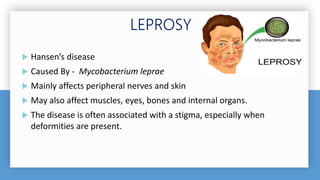
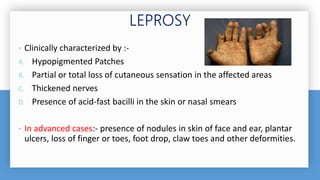
The document discusses leprosy, also known as Hansen's disease, which is caused by Mycobacterium leprae bacteria. It primarily affects the skin and peripheral nerves. Key points include:
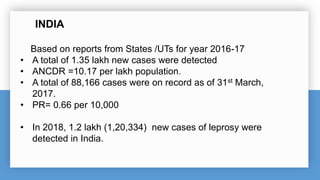
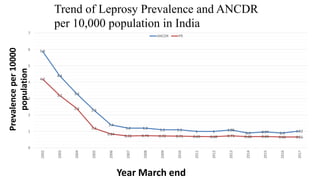
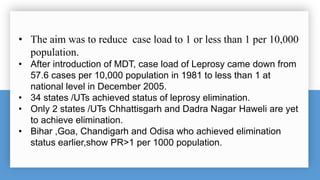
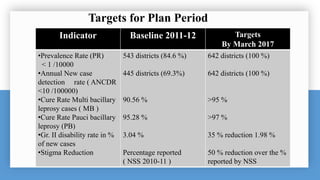
- India detected over 120,000 new leprosy cases in 2018 with a prevalence rate of 0.66 per 10,000 people.
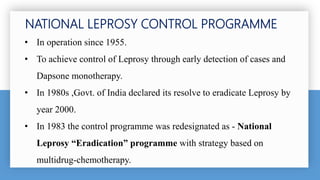
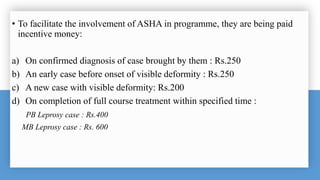
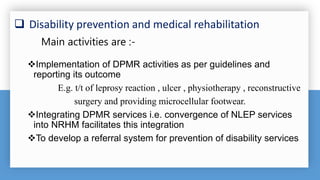
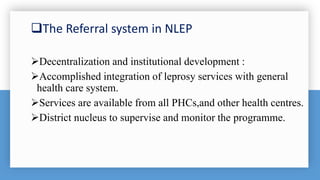
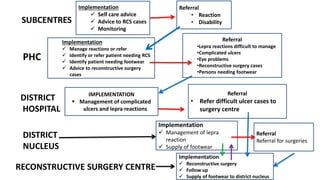
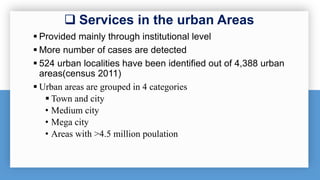
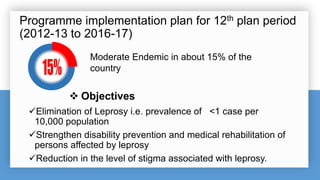
- The National Leprosy Eradication Programme was launched in 1955 and aims to integrate leprosy services into the general healthcare system through early detection, multi-drug therapy treatment, and prevention of disabilities.
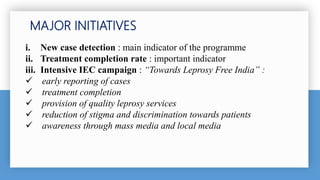
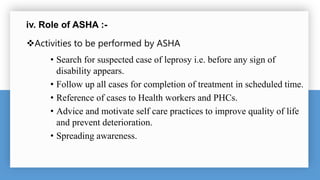
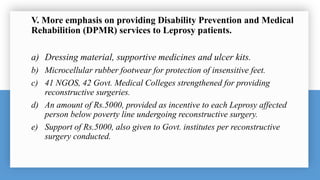
- Major initiatives include intensified case detection, ensuring treatment completion, increasing awareness through media campaigns, and strengthening disability prevention and rehabilitation services.