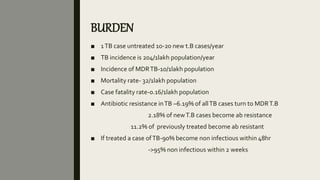
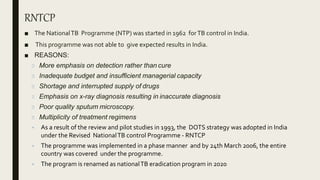
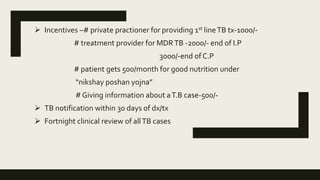
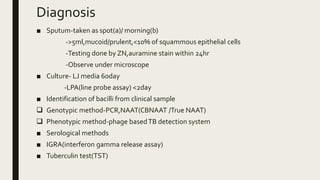
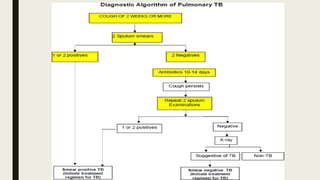
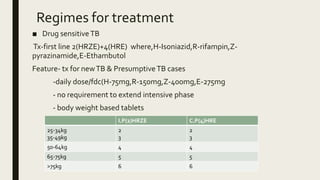
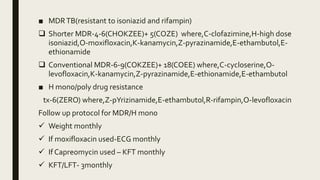
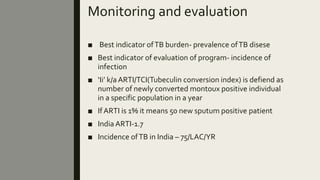
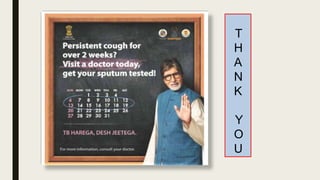
This document summarizes information about the Revised National Tuberculosis Control Program (RNTCP) in India. It discusses the burden of tuberculosis in India, with over 200 new cases per 100,000 people annually. It also outlines the goals and organization of the RNTCP, which aims to decrease TB mortality and cut transmission to eliminate TB in India by 2025. The RNTCP utilizes strategies like active case finding, digital tools for monitoring treatment compliance, and new drug regimens. It provides guidelines for diagnosis using sputum testing and treatment regimens for drug-sensitive and drug-resistant TB, as well as monitoring protocols.