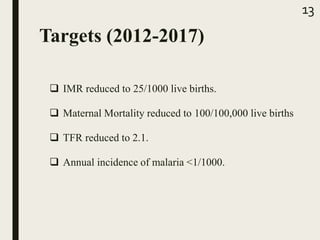
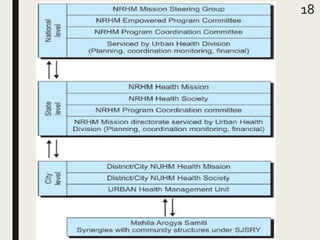
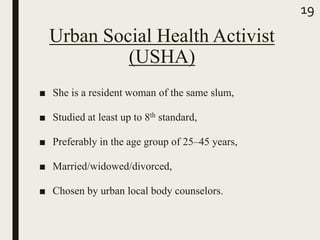
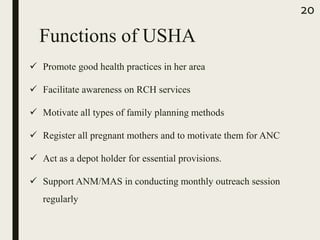
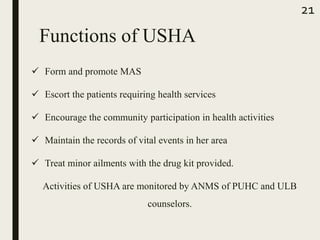
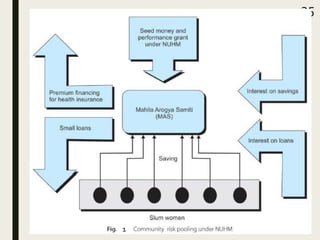
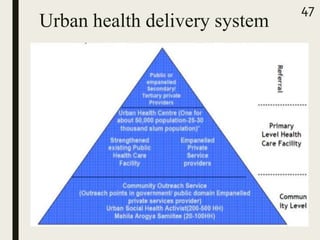
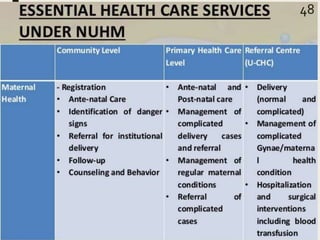
The document discusses India's National Urban Health Mission. The mission aims to provide equitable access to quality health care for the urban poor population as cities are seeing rapid growth. It focuses on improving the efficiency of the public health system and promoting partnerships between government and non-government providers. The mission seeks to meet the health needs of vulnerable groups like slum dwellers through primary health centers, community-based health insurance, and initiatives like the Urban Social Health Activist program. It was established to address the lack of standards and economic barriers to healthcare access faced by many in urban areas.


![References
■ National health mission [online]. 2018 May 23; available from:
URL: nhm.gov.in/nhm/nuhm.html
■ Schemes/ programmes [online]. 2018 June 02; available from: URL:
http://www.uddkar.gov.in
■ Kishore J. National health programs: National Urban Health
Mission. 12th edition
■ Park K. Textbook of Preventive and Social Medicine: National
Health Programs. 24th edition.
■ Textbook of Community medicine with recent advances 4th edition;
Suryakantha (2016); section 4 chapter 17 occupational health pg.
237
■ Bhalwar R. National Urban Health Mission.Textbook of public
health & community medicine 1st edition; AFMC Pune (2009).
49](https://image.slidesharecdn.com/nuhm-180908154356/85/NUHM-49-320.jpg)