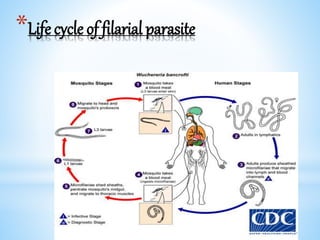
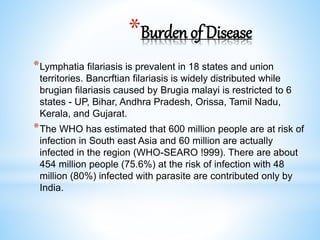
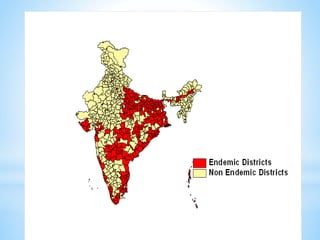
The document discusses lymphatic filariasis (LF), a parasitic disease spread by mosquitoes. It outlines the National Filariasis Control Programme in India, including control strategies like mass drug administration, vector control, and morbidity management. The key goals are to eliminate LF as a public health problem in India by 2021 through annual treatment of at-risk populations and managing symptoms for infected individuals. Significant progress has been made, with over 94 districts qualifying for stopping mass drug administration after validation surveys.