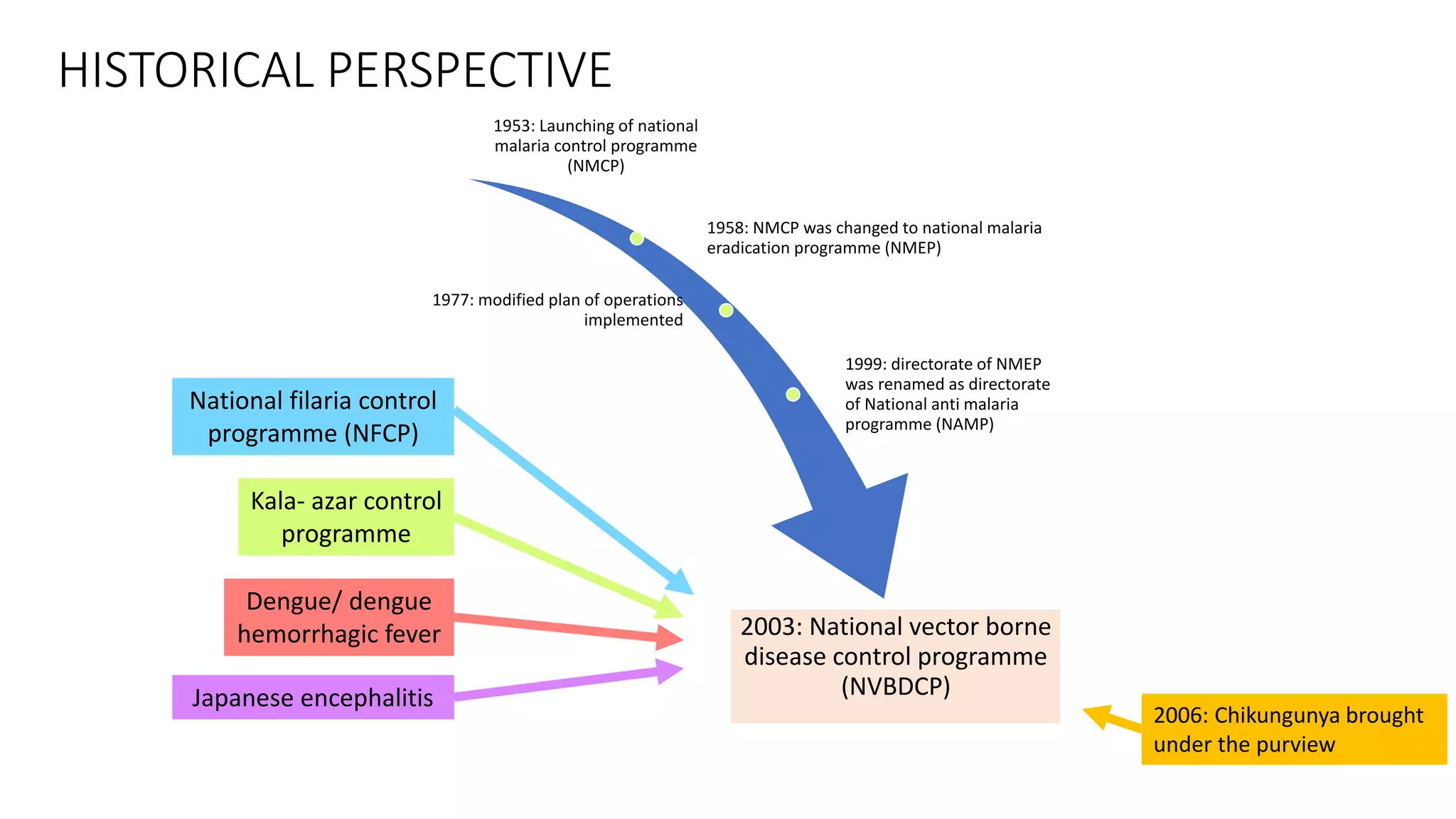
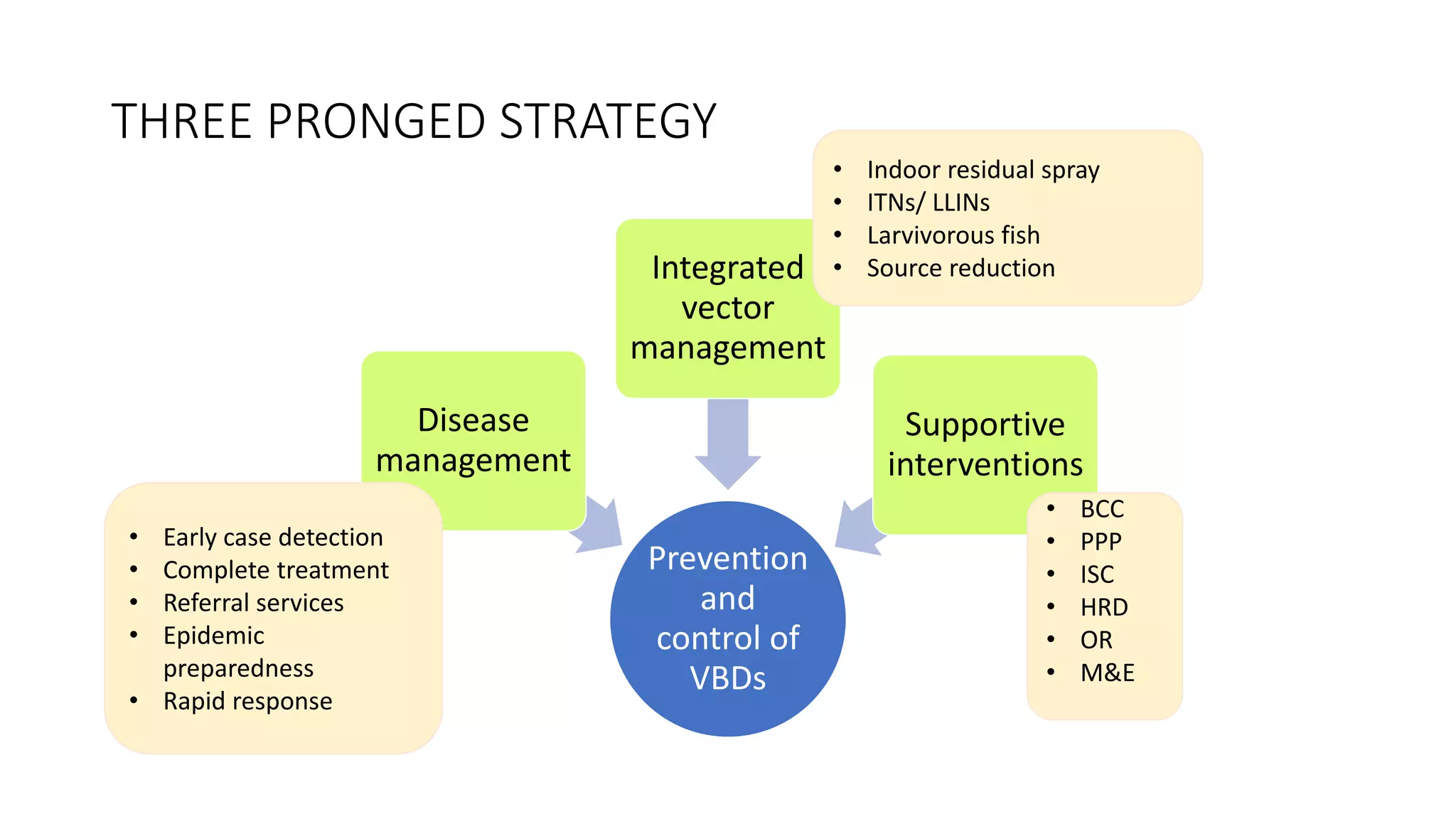
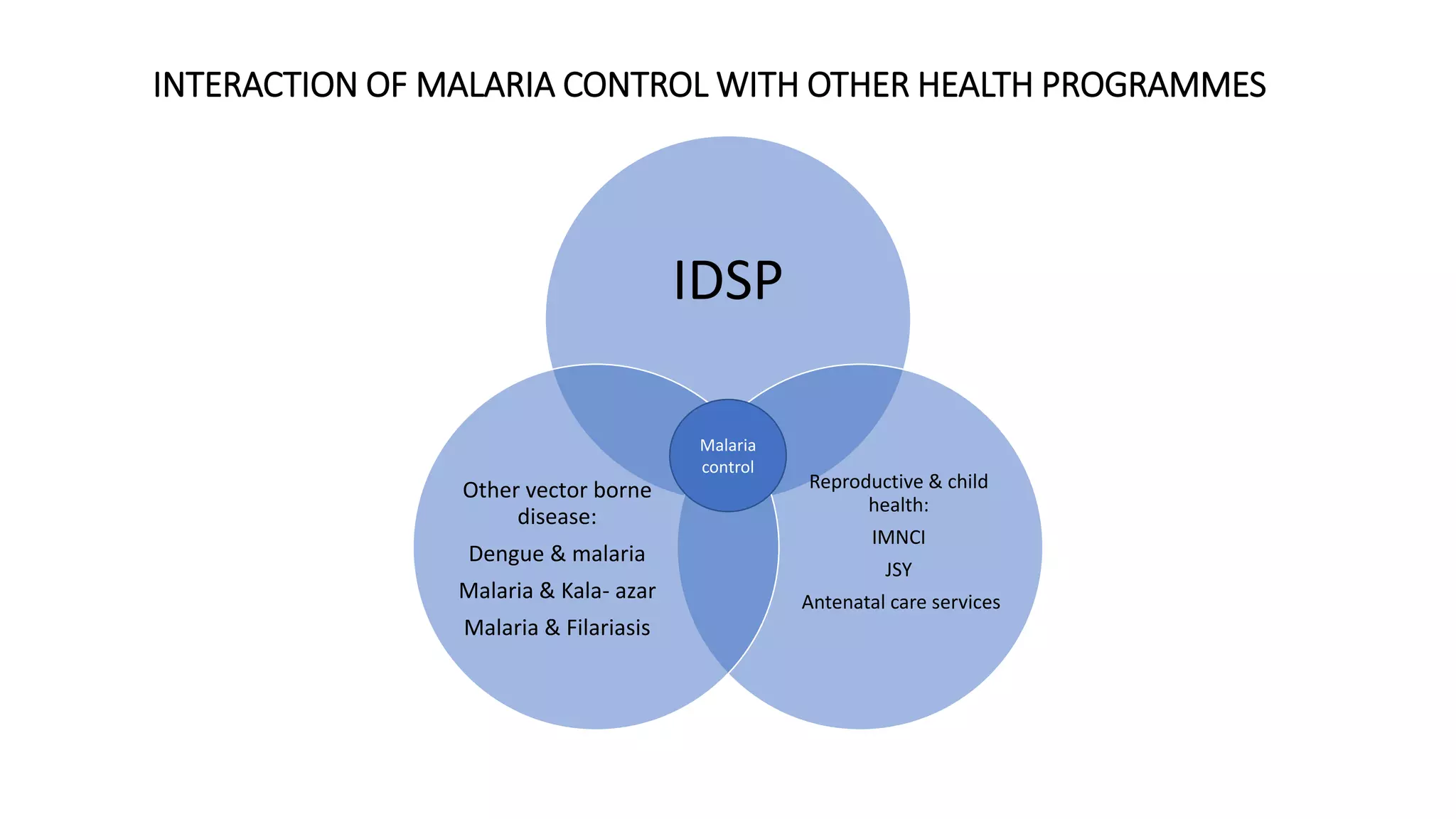
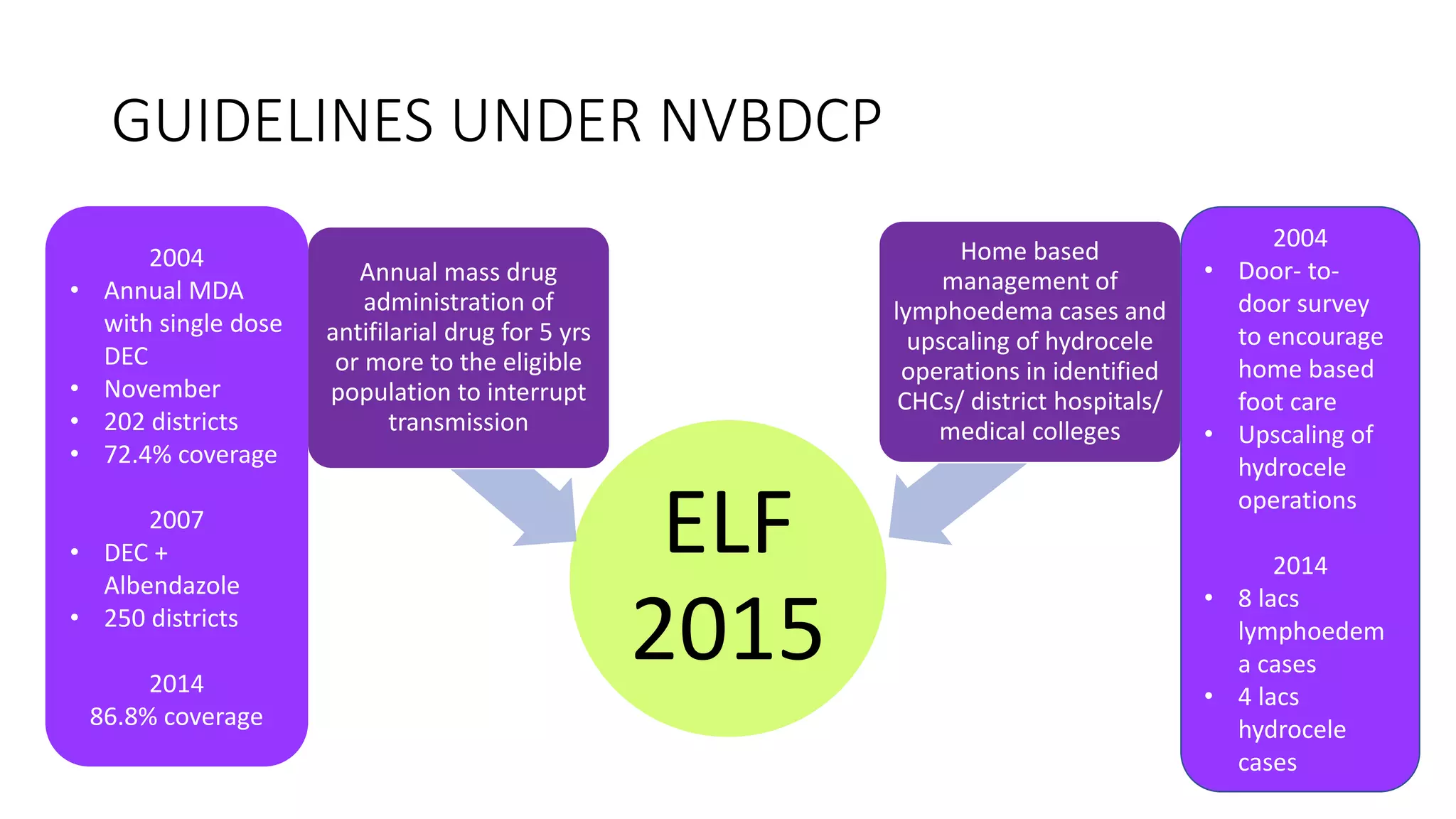
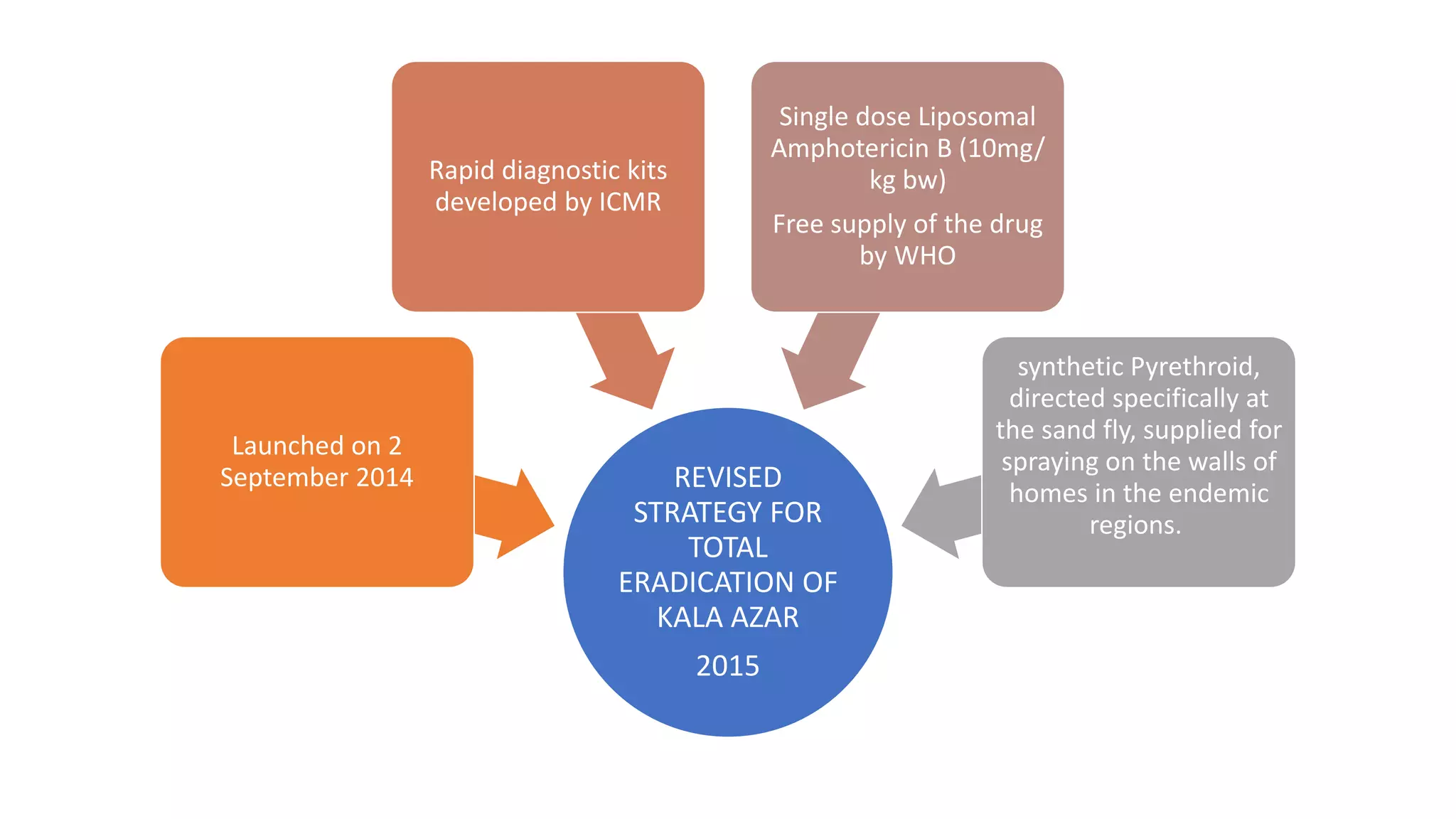
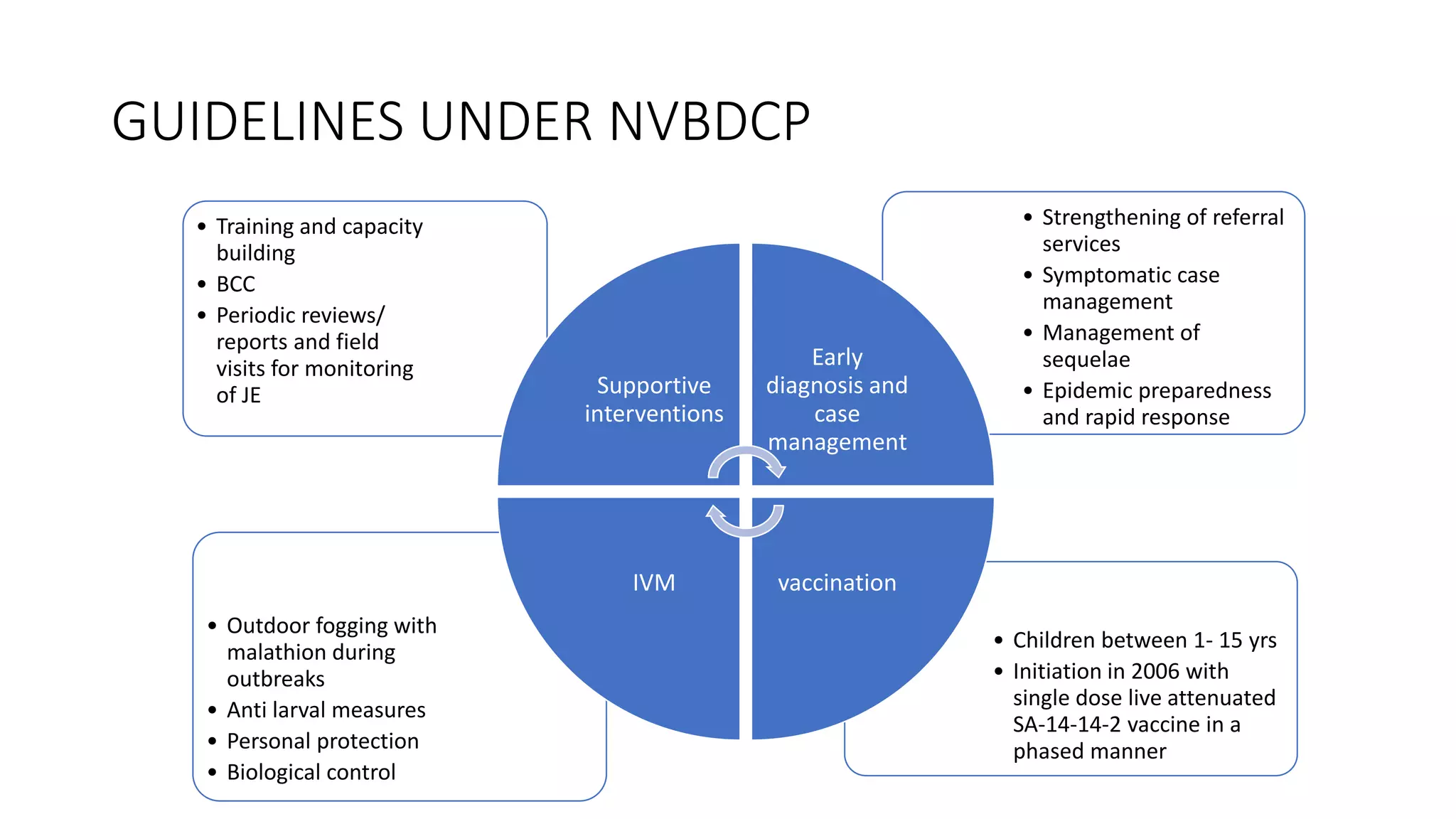
The National Vector Borne Disease Control Programme (NVBDCP) is an umbrella programme under the National Health Mission that aims to control and prevent six vector-borne diseases: malaria, kala-azar, filariasis, dengue, Japanese encephalitis, and chikungunya. The programme focuses on disease management, integrated vector management, and supportive interventions like indoor residual spraying and larvivorous fish. Its goals are to reduce mortality from certain diseases and eliminate kala-azar and filariasis by targeted years. The programme is coordinated by the Directorate of NVBDCP and implemented at national, state, district, and local levels.


















































![REFERENCES
• Park’s textbook of preventive and social medicine, 24th edition.
• www.nvbdcp.gov.in
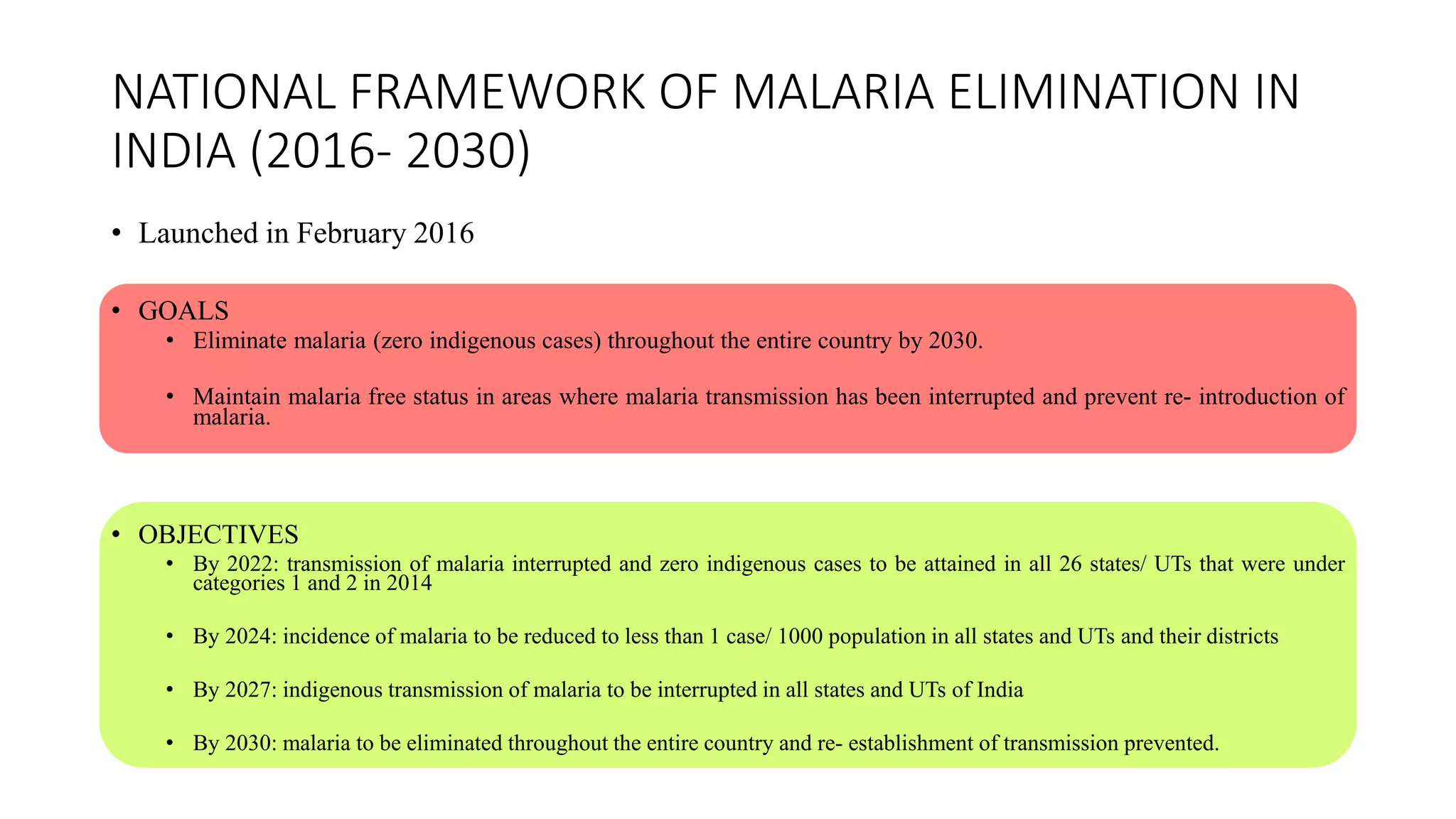
• National Framework for Malaria Elimination in India 2016-2030. Directorate of National Vector Borne
Disease Control Programme (NVBDCP). Ministry of Health & Family Welfare, Government of India. p. 43.
Available from: http://www.nvbdcp.gov.in/malaria [Accessed: 20 February 2018]
• National Vector Borne Disease Control Programme, Directorate General of Health Services, Ministry of
Health & Family Welfare. Government of India. Malaria. Available from: http://www.nvbdcp.gov.in/malaria
[Accessed: February 20, 2018]
• Sabesan, Shanmugavelu & Raju, Hari Kishan & Swaminathan, Subramanian & Srivastava, Pradeep &
Jambulingam, Purushothaman. (2013). Lymphatic Filariasis Transmission Risk Map of India, Based on a
Geo-Environmental Risk Model. Vector borne and zoonotic diseases (Larchmont, N.Y.). 13.
10.1089/vbz.2012.1238.](https://image.slidesharecdn.com/nvbdcp-200212143117/75/NVBDCP-66-2048.jpg)