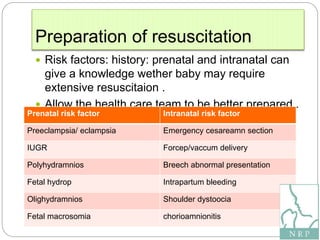
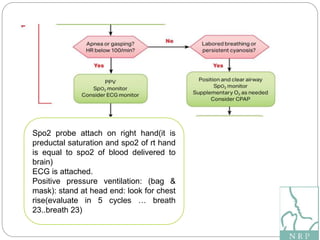
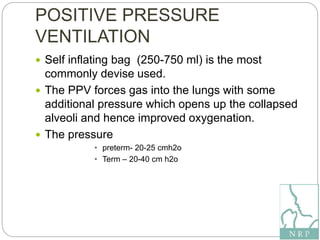
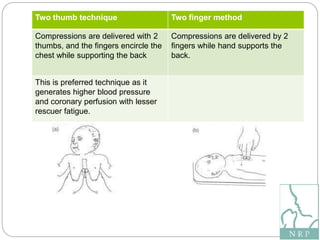
The document outlines the Neonatal Resuscitation Program (NRP) presented by Manisha Thakur, emphasizing the transition of newborns from intra-uterine to extra-uterine life, and the need for immediate assessment and intervention if the baby is not breathing properly. It details key risk factors, essential equipment, and specific resuscitation steps including airway management, positive pressure ventilation, and chest compressions. The program also stresses the importance of post-resuscitation care and monitoring in a neonatal intensive care unit.