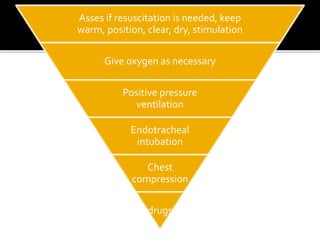
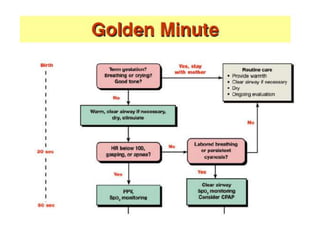
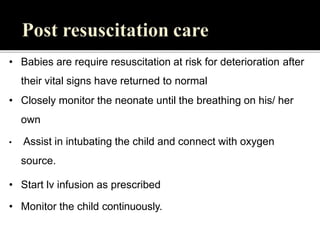
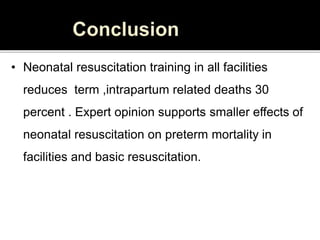
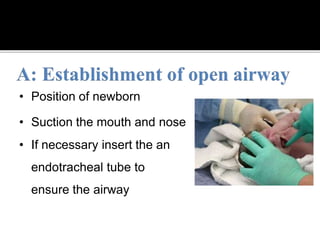
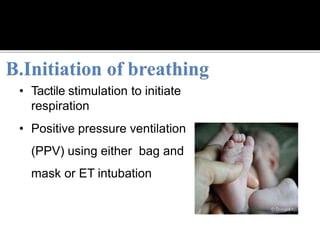
Effective neonatal resuscitation at birth is vital in preventing infant mortality, necessitating comprehensive clinical guidelines tailored for resource-limited settings. The document outlines the essential equipment, procedures, and interventions needed for successful neonatal resuscitation, including temperature maintenance, suctioning, positive pressure ventilation, and chest compressions. It emphasizes the importance of skilled personnel and proper monitoring to ensure the successful stabilization of newborns at risk.




![Started when HR<60 per minute despite adequate
ventilation with 100% oxygen for 30 sec
The pressure is applied to the lower third of the sternum
to depress it ½ to ¾ inches.
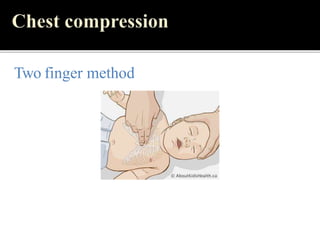
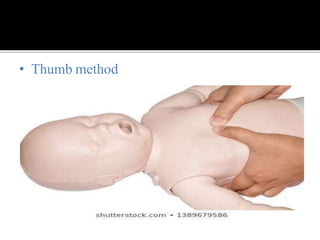
2 techniques:
2 thumb-encircling hands technique
Compression with 2 fingers ,second hand supporting
the back
3:1 ratio::[ 90 comp:30 ventilations]](https://image.slidesharecdn.com/6-240422172624-d7e76958/85/Neonatal-resuscitation-TABC-pptx-43-320.jpg)