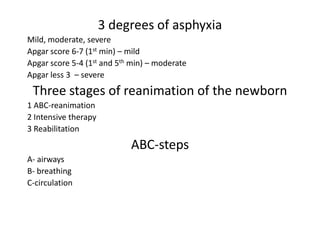
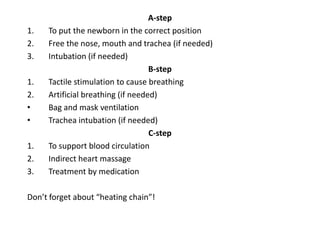
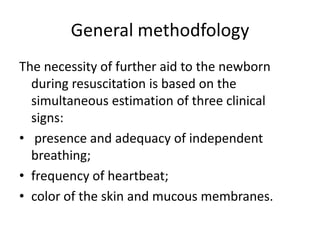
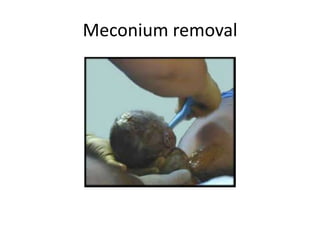
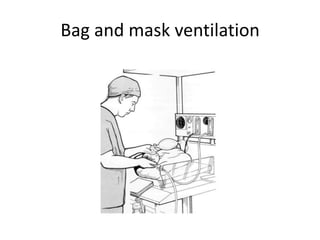
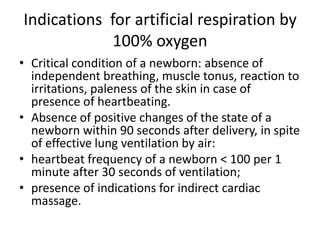
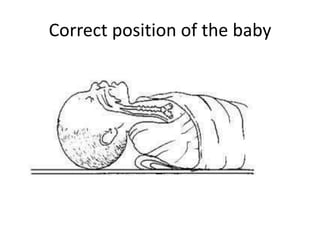
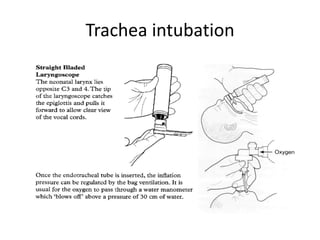
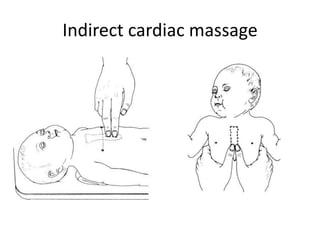
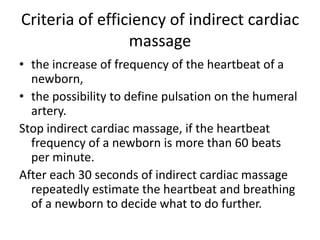
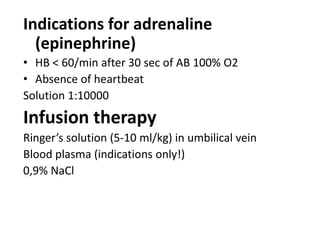
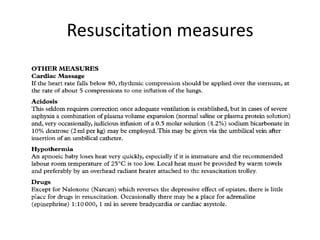
This document provides information on neonatal resuscitation procedures. It discusses asphyxia in newborns and classifies its severity using the Apgar score. The three stages of newborn resuscitation are described as ABC (airway, breathing, circulation) steps. Detailed procedures are outlined for maintaining the airway, initiating breathing support through bag-mask ventilation or intubation, and supporting circulation through cardiac massage and medications if needed. Signs used to assess the newborn and determine the need for further intervention are also summarized. The document emphasizes the importance of re-evaluating the newborn every 30 seconds during resuscitation.